Pregnant women may experience back pain that is localized to the lower back area or radiates into the buttock, thigh, and legs, causing or mimicking sciatica symptoms. The pain may be constant, get worse with activity, interfere with sleep, and/or reduce overall functioning. While the symptoms usually resolve spontaneously after delivery, some conditions may remain as chronic disorders. Women with pre-existing lower back problems are typically at a higher risk of developing pregnancy-related back pain.
During pregnancy, natural anatomic and postural changes cause mechanical challenges to the musculoskeletal system, especially in the lower body. Back pain and pelvic discomfort commonly start between the fifth and seventh month of being pregnant. A small percentage of women may experience pain as early as 4 to 16 weeks. 1 Sabino J, Grauer JN. Pregnancy and low back pain. Curr Rev Musculoskelet Med. 2008;1(2):137-141. doi:10.1007/s12178-008-9021-8
In This Article:
Lower Back Pain in Pregnancy
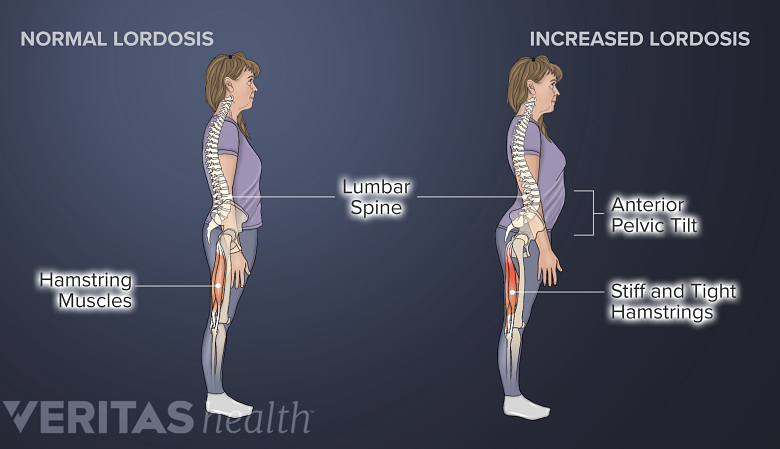
Postural and traumatic changes increase the lordotic curve, disturbing pelvic and hamstring muscle balance.
Mechanical instability in the lumbar spine (lower back) and pelvis commonly results in lower back pain in pregnant women.
- The lumbar spine undergoes compensatory lordosis—an increase in the reverse C-shaped curvature—which causes excess strain on the lumbar joints, muscles, ligaments, and discs.
- The psoas muscle in the hip, which stabilizes the spine and helps in hip and leg movements, is shortened due to the compensatory lordosis, exacerbating the lower back pain symptoms. 2 Chila AG. Foundations of Osteopathic Medicine. Lippincott Williams & Wilkins; 2010.
Lower back pain symptoms may start at any time during pregnancy. These symptoms may feel like:
- A dull ache or sharp, burning pain in the lower back area
- One-sided pain in the right or left area of the lower and/or mid-back
- Pain that radiates into the back of the thigh and leg, and sometimes into the foot (similar to sciatica)
- Foot drop, a condition characterized by the inability to lift the front part of the foot while walking
Sciatica symptoms typically occur if a lower lumbar and/or upper sacral nerve root is impinged in the lower spine due to a lumbar herniated disc, spondylolisthesis, facet joint disorder, or muscle sprain and spasm.
Read more about Common Causes of Back Pain in Pregnancy
Women with a history of back pain, pre-existing lower back disorders, multiple pregnancies, and/or those who are in the younger or older age-groups may be at a higher risk of developing lower back pain in pregnancy. 2 Chila AG. Foundations of Osteopathic Medicine. Lippincott Williams & Wilkins; 2010.
Lower back pain while lying down or sleeping
Pregnancy-related lower back pain that worsens at night may occur as a consequence of the expanding uterus, which applies pressure on a major blood vessel—the vena cava—causing blood vessel congestion in the pelvis and the lumbar spine. 3 Katonis P, Kampouroglou A, Aggelopoulos A, et al. Pregnancy-related low back pain. Hippokratia. 2011;15(3):205-210. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3306025/
Pregnancy Pelvic Pain
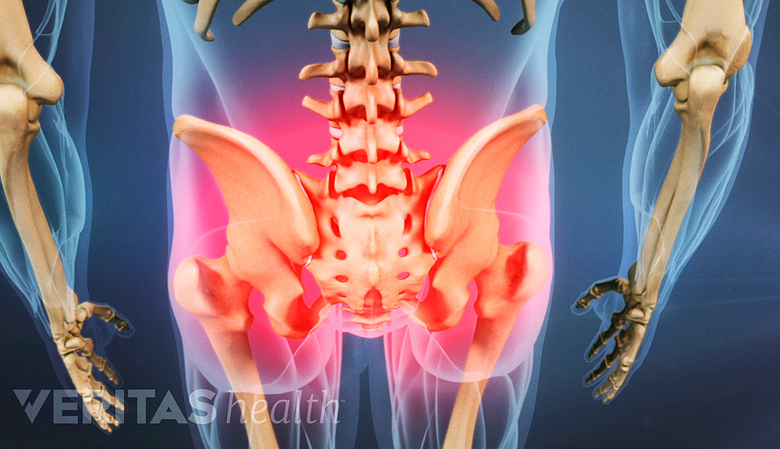
Pregnant women with pelvic pain usually have sacroiliac joint laxity on both sides.
Pelvic changes are normal in pregnancy and help accommodate the growing uterus and facilitate birth.
Pregnant women who experience pelvic pain have different amounts of laxity in their right and left sacroiliac joints, which connect the spine to the pelvis. This difference in joint laxity occurs due to a high concentration of the hormone relaxin that softens the connective tissues and joints. Significant laxity of the sacroiliac joints may cause displacement of the ilium—part of the pelvis that attaches to the sacroiliac joint.
Pain occurs when the shifted ilium is displaced in an unstable position, causing stress on the adjacent tissues. As the body tries to restore the pelvis back into a normal position, the muscles become tense and pull within or around the pelvis. If tension occurs in the pelvic floor muscles or the adductor muscles of the thigh (groin muscles that help pull the legs together) severe pain may be felt. 4 Rost C. Relieving Pelvic Pain During and After Pregnancy, How Women Can Heal Chronic Pelvic Instability. Hunter House; 2013.
Posterior pelvic pain is common during pregnancy and may affect up to 76% of pregnant women. This pain may also be experienced for several years after childbirth in 5% to 8.5% of new mothers. 5 Kanakaris NK, Roberts CS, Giannoudis PV. Pregnancy-related pelvic girdle pain: an update. BMC Med. 2011;9:15. Published 2011 Feb 15. doi:10.1186/1741-7015-9-15 Doctors may also refer to this pain as pelvic girdle pain or symphysis pubis dysfunction.
Typical features of posterior pelvic pain include:
- Pain that may feel like a stabbing, dull, shooting, and/or burning sensation in the back of the pelvic area
- Pain that may extend into the buttock and radiate to the groin and back of the thigh
- Pain that may mimic sciatica, but unlike sciatica, is often impossible to locate precisely and may change in type or area(s) affected as pregnancy progresses 5 Kanakaris NK, Roberts CS, Giannoudis PV. Pregnancy-related pelvic girdle pain: an update. BMC Med. 2011;9:15. Published 2011 Feb 15. doi:10.1186/1741-7015-9-15
Women with a history of lower back pain before pregnancy and/or those with physically demanding jobs that require them to stand for extended periods are at a greater risk of developing pelvic pain while pregnant. 4 Rost C. Relieving Pelvic Pain During and After Pregnancy, How Women Can Heal Chronic Pelvic Instability. Hunter House; 2013.
Thigh Pain in Pregnancy
Temporary compression, pulling, and/or loss of blood supply to a peripheral nerve may occur in the thigh during pregnancy. The swelling of soft tissues and pressure from the growing uterus may add additional pressure on these nerves.
Thigh pain may occur under these circumstances when the lateral femoral cutaneous nerve gets compressed. This nerve provides sensation to the waist area and the front and side of the thigh. 2 Chila AG. Foundations of Osteopathic Medicine. Lippincott Williams & Wilkins; 2010.
Compression of the lateral femoral cutaneous nerve results in a condition called meralgia paresthetica, which causes one or more of the following symptoms, typically on one side of the body 6 Cheatham SW, Kolber MJ, Salamh PA. Meralgia paresthetica: a review of the literature. Int J Sports Phys Ther. 2013;8(6):883-93. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3867081/ :
- Burning or achy pain in the outer side and/or front of the thigh
- A cold, icy feeling in different parts of the thigh
- Buzzing or vibrations (such as from a cell phone) in the thigh
Meralgia paresthetica pain increases with activity, such as while standing or walking, and alleviates when sitting. 6 Cheatham SW, Kolber MJ, Salamh PA. Meralgia paresthetica: a review of the literature. Int J Sports Phys Ther. 2013;8(6):883-93. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3867081/
Pregnancy Back and Hip Pain
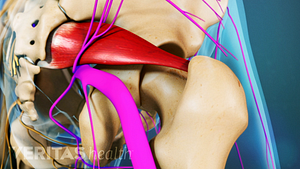
Changes in the lower back and pelvis during pregnancy are a risk factor for hip pain.
The hip may become painful during pregnancy due to changes in the lower back and pelvis. Different parts of the hip may be affected, resulting in a range of potential disorders in this region. 2 Chila AG. Foundations of Osteopathic Medicine. Lippincott Williams & Wilkins; 2010.
Transient osteoporosis
A rare condition, transient osteoporosis, may occur due to weight-bearing in the third trimester of pregnancy. This condition causes weakening of the hip bone and results in acute pain with limited motion in the hip. Pain in transient osteoporosis typically comes on suddenly and is aggravated when bearing weight, such as while standing or walking. Women with this condition typically walk by taking short steps to avoid pain (antalgic gait). 2 Chila AG. Foundations of Osteopathic Medicine. Lippincott Williams & Wilkins; 2010.
Avascular necrosis of the femoral head
Biological changes in pregnancy resulting in high levels of natural steroids, including adrenocorticoid, estrogen, and progesterone hormones, combined with weight gain, may cause increased joint pressure and muscle strain in the hip. These changes may result in a condition called avascular necrosis of the upper part (head) of the femoral bone (thigh bone). The condition causes destruction of bone tissue in the femoral head due to lack of blood supply. 2 Chila AG. Foundations of Osteopathic Medicine. Lippincott Williams & Wilkins; 2010.
The symptoms of avascular necrosis of the femoral head start around the third trimester and include 2 Chila AG. Foundations of Osteopathic Medicine. Lippincott Williams & Wilkins; 2010. :
- Pain that is felt deep in the groin (inner thigh)
- Radiating and referred pain to the lower back, thigh, and/or knee
The symptoms are exacerbated on bearing weight, such as while standing and/or walking.
Lower Back and Abdominal Pain with Cramping
Sudden onset of severe abdominal pain and cramping may indicate a ruptured ectopic pregnancy. In this condition, the egg fertilizes and grows in a place other than the uterus, most commonly inside the fallopian tube, which ruptures due to the growing size of the fertilized egg. 7 Dalsgaard Jensen T, Penninga L. Non-operative treatment of ruptured ectopic pregnancy. BMJ Case Rep. 2016;2016:bcr2016215311. Published 2016 Jun 13. doi:10.1136/bcr-2016-215311
The symptoms of a ruptured ectopic pregnancy may also include severe lower back and/or groin pain. This condition is a medical emergency and must be treated with surgical intervention on an urgent basis.
Back Labor Pain
Pain during active labor is caused by contraction of the muscles of the uterus and is similar to an intense menstrual cramp. Labor pain typically comes-and-goes and gradually increases in intensity.
Some women may experience severe lower back pain during labor, often called back labor. Back labor pain becomes intense between contractions and remains steady between contractions. This pain may occur when the baby is mispositioned in a way that the back of the baby's head presses against the mother's back (occiput posterior position).
Back pain while being pregnant typically resolves on its own after delivery. Pain that suddenly becomes severe, lasts for several weeks, worsens over time, is accompanied by neurologic deficits, and/or is not relieved by rest or treatment must be evaluated by a doctor without delay.
- 1 Sabino J, Grauer JN. Pregnancy and low back pain. Curr Rev Musculoskelet Med. 2008;1(2):137-141. doi:10.1007/s12178-008-9021-8
- 2 Chila AG. Foundations of Osteopathic Medicine. Lippincott Williams & Wilkins; 2010.
- 3 Katonis P, Kampouroglou A, Aggelopoulos A, et al. Pregnancy-related low back pain. Hippokratia. 2011;15(3):205-210. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3306025/
- 4 Rost C. Relieving Pelvic Pain During and After Pregnancy, How Women Can Heal Chronic Pelvic Instability. Hunter House; 2013.
- 5 Kanakaris NK, Roberts CS, Giannoudis PV. Pregnancy-related pelvic girdle pain: an update. BMC Med. 2011;9:15. Published 2011 Feb 15. doi:10.1186/1741-7015-9-15
- 6 Cheatham SW, Kolber MJ, Salamh PA. Meralgia paresthetica: a review of the literature. Int J Sports Phys Ther. 2013;8(6):883-93. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3867081/
- 7 Dalsgaard Jensen T, Penninga L. Non-operative treatment of ruptured ectopic pregnancy. BMJ Case Rep. 2016;2016:bcr2016215311. Published 2016 Jun 13. doi:10.1136/bcr-2016-215311