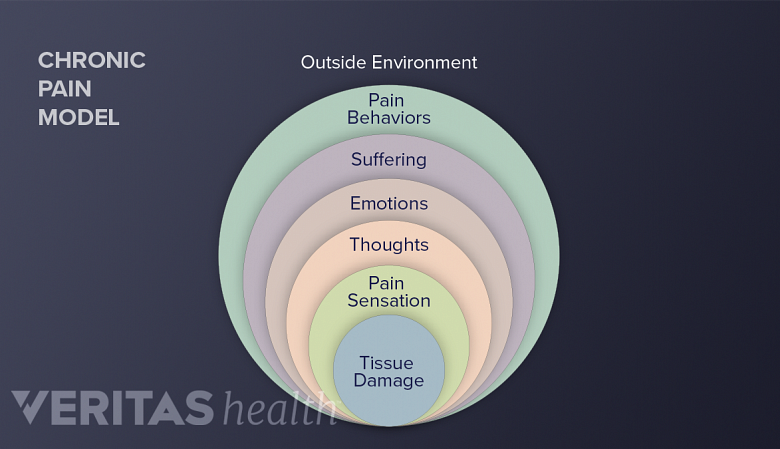
A number of factors play a role in the experience of chronic pain. It may be helpful to view this model to conceptualize the complicated nature of this common condition.
In This Article:
Tissue damage. This is simply the tissue injury or damage that initially started the pain. The tissue damage causes input to the nervous system (the pain signal). This is also termed “nociceptive input.”
See How Soft Tissue Injuries Cause Neck Strain
Pain sensation. In the simplest terms of this model, pain sensation is the actual perception that occurs in the brain after the nerve signal (due to nociception) travels from the periphery to the central nervous system. Pain sensation is experienced in the brain, while nociception occurs at the site of injury.
Thoughts. Cognitions or thoughts occur in higher brain centers and are an assessment of the pain sensation signal coming into the nervous system as well as events surrounding it. These thoughts can be conscious or unconscious and will greatly influence how the pain signal is perceived. For instance, general body aches and stiffness are perceived as "good pain" when these occur after a vigorous exercise session, whereas they are perceived as "bad pain" when related to a medical condition, such as fibromyalgia.
Emotions. The emotional aspect of pain is a person’s response to thoughts about the pain. If you believe (thoughts) the pain is a serious threat (e.g. a tumor), then emotional responses will include fear, depression, and anxiety, among others. Conversely if you believe the pain is not a threat, then the emotional response will be negligible.
Suffering. The term “suffering” is often used as a synonym for “pain” even though they are theoretically and conceptually distinct. For instance, a broken bone may cause pain without suffering (since the person knows the pain is not deadly and the bone will heal). In contrast, bone pain due to a tumor may cause the same pain as a break but the suffering will be much greater due to the “meaning” behind the pain (this tumor could be life-threatening). Suffering is very closely tied to the emotional aspect of pain.
See 4 Tips to Help Cope With Chronic Pain and Depression
Pain behaviors. Pain behaviors are defined as things people do when they suffer or are in pain. These are behaviors that others observe as typically indicating pain, such as talking about the pain, grimacing, limping, moving slowly, and taking pain medicine. Pain behaviors are in response to all the other factors in the pain system model (tissue damage, pain sensation, thoughts, emotions, and suffering). Pain behaviors are also affected by previous life experiences, expectations, and cultural influences in terms of how the pain is expressed. Interestingly, pain behaviors are also affected by the outside environment, such as how others respond.
Psychosocial environment. The psychosocial environment includes all of the environments in which an individual lives, works, and plays. Research has consistently shown that these environments influence how much a person will show pain behaviors.