A foot drop typically occurs due to weakness in specific muscles of the leg. These muscles include 1 Daniels SP, Feinberg JH, Carrino JA, Behzadi AH, Sneag DB. MRI of Foot Drop: How We Do It. Radiology. 2018;289(1):9-24. doi:10.1148/radiol.2018172634 :
- Tibialis anterior
- Extensor hallucis longus
- Extensor digitorum longus
The tendons of these muscles insert into the bones of the foot and/or toes, resulting in foot weakness and difficulty in lifting the foot and/or toes upward and in other directions.
Weakness in these muscles may be caused by neurological or muscular disorders. A few common causes are discussed below.
In This Article:
Neurological Causes of Foot Drop
Nerves in the lower back and/or leg may be pinched or may get damaged and degenerated, causing foot drop.
Radiculopathy
Spinal nerve root irritation in the lumbar and/or sacral spine causes foot drop.
Irritation or compression of spinal nerve roots in the lumbar and/or sacral spine may cause foot drop due to radiculopathy. The symptoms of radiculopathy typically include weakness, pain, tingling, and/or numbness in the skin and/or muscles supplied by the affected nerve.
Foot drop is commonly caused by radiculopathy of the L5 nerve root. Sometimes, radiculopathy from L4 and/or S1 may also cause foot drop. 2 Liu K, Zhu W, Shi J, et al. Foot drop caused by lumbar degenerative disease: clinical features, prognostic factors of surgical outcome and clinical stage. PLoS One. 2013;8(11):e80375. Published 2013 Nov 5. doi:10.1371/journal.pone.0080375 Radiculopathy occurs due to:
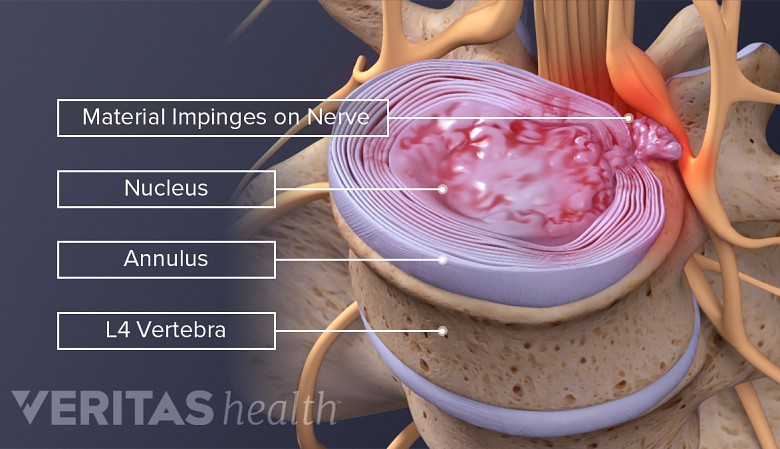
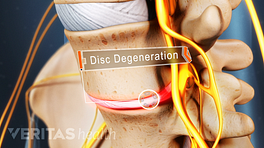
- Herniated disc. Bulging or leaking of the inner gelatinous contents of an intervertebral disc causing mechanical compression or chemical irritation of the adjacent nerve root.
- Foraminal spinal stenosis. Narrowing of the small bony openings for spinal nerves on the side of the spine due to abnormal bone growth (bone spurs) or degenerative changes, causing pressure on the nerve roots.
- Spondylolisthesis. Slipping of one vertebra over the adjacent lower vertebra due to degeneration or stress may compress a nerve root in between the vertebrae.
The symptoms of radiculopathy typically affect one foot, sometimes, both feet may be affected when nerve roots on either side of the spine are compressed, such as in spondylolisthesis or severe herniation.
Neuropathy
When a nerve is compressed, damaged, or degenerated along its path, it is called neuropathy. Foot drop commonly occurs due to neuropathy of the following nerves:
- Common peroneal nerve. Neuropathy of this nerve may occur due to trauma to the knee, fracture of the fibula bone, pressure from tight boots or plaster, excessive weight loss, ankle sprain, or as a complication of knee surgery. 3 Craig A, Richardson JK. Localized peripheral neuropathies. In: A Comprehensive Guide to Geriatric Rehabilitation. Elsevier; 2014:233-241. doi:10.1016/b978-0-7020-4588-2.00033-4 , 4 Common Peroneal Nerve Dysfunction: MedlinePlus Medical Encyclopedia. MedlinePlus, U.S. National Library of Medicine, medlineplus.gov/ency/article/000791.htm. Reviewed Aug 07, 2017. Accessed: July 22, 2019.
- Deep peroneal nerve. Neuropathy of this nerve may occur due to increased pressure within the muscle bundles of the leg or compartment syndrome, fracture of the leg’s tibial bone, or internal bleeding within the leg. 3 Craig A, Richardson JK. Localized peripheral neuropathies. In: A Comprehensive Guide to Geriatric Rehabilitation. Elsevier; 2014:233-241. doi:10.1016/b978-0-7020-4588-2.00033-4
- Sciatic nerve. Neuropathy of the sciatic nerve may occur due to repeated injections in the hip, a complication of hip surgery, or trauma to the hip and/or pelvis. 3 Craig A, Richardson JK. Localized peripheral neuropathies. In: A Comprehensive Guide to Geriatric Rehabilitation. Elsevier; 2014:233-241. doi:10.1016/b978-0-7020-4588-2.00033-4
Neuropathy of the common peroneal nerve occurs more frequently compared to other nerves in the leg.3 This nerve runs superficially near the knee, covered by skin and a thin layer of underlying tissue—making it vulnerable to direct injury. 5 Lavelle JM, Mckeigue ME. Musculoskeletal dysfunction and drop foot: diagnosis and management using osteopathic manipulative medicine. J Am Osteopath Assoc. 2009;109(12):648-50.
Neuropathy may also occur due to systemic and metabolic conditions, including:
- Autoimmune disorders such as multiple sclerosis 6 Larson RD, Cantrell GS, Farrell JW, Lantis DJ, Pribble BA. Assessment, Consequence, and Clinical Implication of Asymmetry. In: Nutrition and Lifestyle in Neurological Autoimmune Diseases. Elsevier; 2017:127-134. doi:10.1016/b978-0-12-805298-3.00013-x or polyarteritis nodosa 4 Common Peroneal Nerve Dysfunction: MedlinePlus Medical Encyclopedia. MedlinePlus, U.S. National Library of Medicine, medlineplus.gov/ency/article/000791.htm. Reviewed Aug 07, 2017. Accessed: July 22, 2019.
- Systemic disorders such as Diabetes mellitus 4 Common Peroneal Nerve Dysfunction: MedlinePlus Medical Encyclopedia. MedlinePlus, U.S. National Library of Medicine, medlineplus.gov/ency/article/000791.htm. Reviewed Aug 07, 2017. Accessed: July 22, 2019. or vasculitis 7 Bertorini TE. A Man with Recurrent Foot Drop*. In: Neuromuscular Case Studies. Elsevier; 2008:386-392. doi:10.1016/b978-0-7506-7332-7.50068-4
- Genetic disorders such as Charcot-Marie-Tooth disease 4 Common Peroneal Nerve Dysfunction: MedlinePlus Medical Encyclopedia. MedlinePlus, U.S. National Library of Medicine, medlineplus.gov/ency/article/000791.htm. Reviewed Aug 07, 2017. Accessed: July 22, 2019. or hereditary neuropathy with liability to pressure palsies (HNPP) 7 Bertorini TE. A Man with Recurrent Foot Drop*. In: Neuromuscular Case Studies. Elsevier; 2008:386-392. doi:10.1016/b978-0-7506-7332-7.50068-4
- Alcohol, when used in excess may damage the nerves 4 Common Peroneal Nerve Dysfunction: MedlinePlus Medical Encyclopedia. MedlinePlus, U.S. National Library of Medicine, medlineplus.gov/ency/article/000791.htm. Reviewed Aug 07, 2017. Accessed: July 22, 2019.
Neuropathy from these conditions may affect nerves in both legs, resulting in bilateral foot drop.
See Understanding Neuropathy Symptoms
Central nervous system causes
While very rare, a tumor, blocked blood vessel, or bleeding in the brain may cause foot drop. These lesions may compress a specific area of the brain (motor cortex) that is associated with leg function. 8 Dolev A, Robinson D, Yassin M. A Central Nervous System Tumor Mimicking a Lumbar Spine Pathology Causing Acute Foot Drop: A Case Report. J Orthop Case Rep. 2018;8(5):78–81. doi:10.13107/jocr.2250-0685.1222
Muscular Causes of Foot Drop
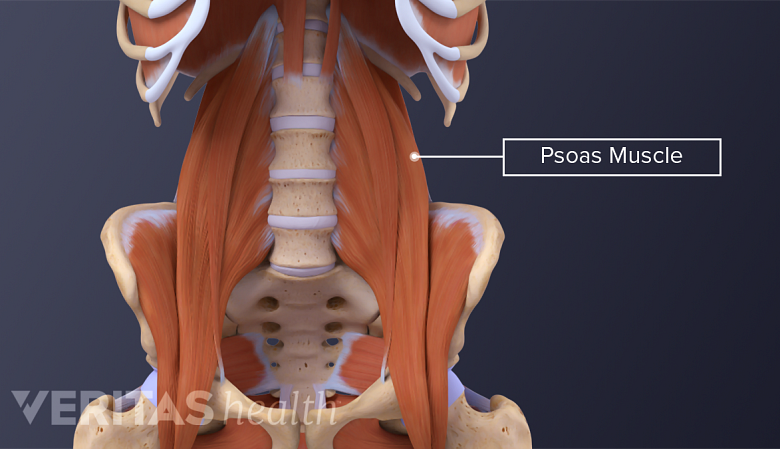
Loss of function in hip flexor muscles may cause foot drop.
Muscular disorders or conditions that lead to progressive muscular weakness such as myotonic dystrophy may cause foot drop. 9 Katirji B. Case 8. In: Electromyography in Clinical Practice. Elsevier; 2007:143-156. doi:10.1016/b978-0-323-02899-8.50017-3 Specifically, loss of function in the following group of muscles may lead to foot drop 10 Chaitow L, DeLany J. Gait analysis. In: Clinical Application of Neuromuscular Techniques, Volume 2. Elsevier; 2011:61-84. doi:10.1016/b978-0-443-06815-7.00003-6 :
- Pretibial or peroneal muscles on the front and side of the leg
- Hip flexor muscles
While rare, infections such as poliomyelitis (polio) can also cause muscular weakness and/or paralysis leading to foot drop. 9 Katirji B. Case 8. In: Electromyography in Clinical Practice. Elsevier; 2007:143-156. doi:10.1016/b978-0-323-02899-8.50017-3
Risk Factors for Foot Drop
Occupations such as melon or strawberry picking or jobs that require prolonged kneeling or squatting, such as flooring or tiling may cause foot drop due to nerve compression. Habitual postures such as regular crossing of legs may lead to peroneal nerve compression near the knee and is a risk factor for foot drop.
While foot drop may be a temporary symptom of an underlying cause, sometimes it can be permanent. The symptoms usually improve with prompt treatment.
- 1 Daniels SP, Feinberg JH, Carrino JA, Behzadi AH, Sneag DB. MRI of Foot Drop: How We Do It. Radiology. 2018;289(1):9-24. doi:10.1148/radiol.2018172634
- 2 Liu K, Zhu W, Shi J, et al. Foot drop caused by lumbar degenerative disease: clinical features, prognostic factors of surgical outcome and clinical stage. PLoS One. 2013;8(11):e80375. Published 2013 Nov 5. doi:10.1371/journal.pone.0080375
- 3 Craig A, Richardson JK. Localized peripheral neuropathies. In: A Comprehensive Guide to Geriatric Rehabilitation. Elsevier; 2014:233-241. doi:10.1016/b978-0-7020-4588-2.00033-4
- 4 Common Peroneal Nerve Dysfunction: MedlinePlus Medical Encyclopedia. MedlinePlus, U.S. National Library of Medicine, medlineplus.gov/ency/article/000791.htm. Reviewed Aug 07, 2017. Accessed: July 22, 2019.
- 5 Lavelle JM, Mckeigue ME. Musculoskeletal dysfunction and drop foot: diagnosis and management using osteopathic manipulative medicine. J Am Osteopath Assoc. 2009;109(12):648-50.
- 6 Larson RD, Cantrell GS, Farrell JW, Lantis DJ, Pribble BA. Assessment, Consequence, and Clinical Implication of Asymmetry. In: Nutrition and Lifestyle in Neurological Autoimmune Diseases. Elsevier; 2017:127-134. doi:10.1016/b978-0-12-805298-3.00013-x
- 7 Bertorini TE. A Man with Recurrent Foot Drop*. In: Neuromuscular Case Studies. Elsevier; 2008:386-392. doi:10.1016/b978-0-7506-7332-7.50068-4
- 8 Dolev A, Robinson D, Yassin M. A Central Nervous System Tumor Mimicking a Lumbar Spine Pathology Causing Acute Foot Drop: A Case Report. J Orthop Case Rep. 2018;8(5):78–81. doi:10.13107/jocr.2250-0685.1222
- 9 Katirji B. Case 8. In: Electromyography in Clinical Practice. Elsevier; 2007:143-156. doi:10.1016/b978-0-323-02899-8.50017-3
- 10 Chaitow L, DeLany J. Gait analysis. In: Clinical Application of Neuromuscular Techniques, Volume 2. Elsevier; 2011:61-84. doi:10.1016/b978-0-443-06815-7.00003-6