Foot drop can be challenging to diagnose due to several potential causes with overlapping symptoms. 1 Daniels SP, Feinberg JH, Carrino JA, Behzadi AH, Sneag DB. MRI of Foot Drop: How We Do It. Radiology. 2018;289(1):9-24. doi:10.1148/radiol.2018172634 The diagnostic process for foot drop includes conducting a physical exam and reviewing the medical history. As needed, one or more diagnostic tests may be required.
In This Article:
Physical Examination and Medical History
A positive Tinel's sign indicates foot drop due to peroneal nerve compression.
Conducting a physical exam and reviewing the medical history helps a doctor to identify the pattern of weakness, numbness, and/or pain in the foot and leg.
Physical exam
During a physical exam, the doctor may check for:
- Pain and numbness in the toes, feet, and leg
- Response to certain stimuli, such as gently pressing the toes or calf region
The doctor may conduct certain clinical tests to check for weakness in the hip, leg, and foot muscles. These tests may include the doctor moving the foot, leg, and thigh in different directions to check the muscles of the ankle, leg, knee, and hip.
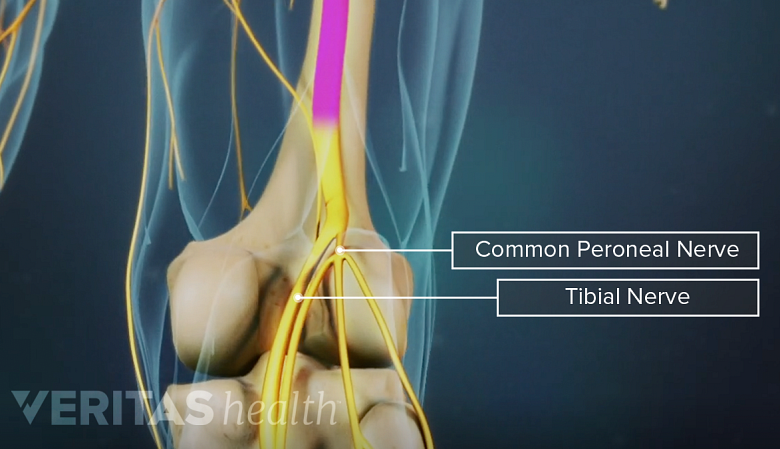
Tinel’s sign test
A positive Tinel’s sign is usually seen in case of peroneal nerve compression. 2 Craig A, Richardson JK. Localized peripheral neuropathies. In: A Comprehensive Guide to Geriatric Rehabilitation. Elsevier; 2014:233-241. doi:10.1016/b978-0-7020-4588-2.00033-4 Tinel’s sign is a tingling or pins-and-needles type of sensation that is perceived when the affected nerve is tapped lightly. Testing for Tinel’s sign in foot drop is done by tapping the side of the knee to check the peroneal nerve.
Medical history
A medical history may include the doctor reviewing the following:
- The onset of weakness and other symptoms
- Concomitant medical conditions, such as diabetes or multiple sclerosis
- Trauma or injury to the back, hip, leg, or foot
- Decreased strength in other parts of the body
If foot drop is suspected, diagnostic tests may be required to check the muscle and nerve tissues in the affected leg. Tests may also be conducted to check for systemic conditions, such as diabetes or genetic disorders that may affect the nerves.
Electrodiagnostic Testing for Foot Drop
The first-line test for checking nerve and muscle health in the legs is electrodiagnostic testing, which includes nerve conduction study and electromyography. 1 Daniels SP, Feinberg JH, Carrino JA, Behzadi AH, Sneag DB. MRI of Foot Drop: How We Do It. Radiology. 2018;289(1):9-24. doi:10.1148/radiol.2018172634
Nerve conduction study
This test involves the assessment of motor and sensory nerve conduction using electrodes that are taped on the skin of the leg. The tests help to identify if the nerves in the leg are damaged or demyelinated (loss of the outer covering of the nerve or myelin sheath). 1 Daniels SP, Feinberg JH, Carrino JA, Behzadi AH, Sneag DB. MRI of Foot Drop: How We Do It. Radiology. 2018;289(1):9-24. doi:10.1148/radiol.2018172634
Watch Video: What is EMG/NCS?
Electromyography (EMG)
In an EMG test, small needles are inserted in the affected muscles to test the electrical activity. 1 Daniels SP, Feinberg JH, Carrino JA, Behzadi AH, Sneag DB. MRI of Foot Drop: How We Do It. Radiology. 2018;289(1):9-24. doi:10.1148/radiol.2018172634 The electric signals are displayed on a monitor, which are interpreted by a doctor.
Magnetic Resonance Neurography
An advanced and detailed medical imaging technique for nerves includes magnetic resonance (MR) neurography, which may be more effective than electrodiagnostic testing. 1 Daniels SP, Feinberg JH, Carrino JA, Behzadi AH, Sneag DB. MRI of Foot Drop: How We Do It. Radiology. 2018;289(1):9-24. doi:10.1148/radiol.2018172634 , 3 Lopes FCR. Neurography - a new look at the peripheral nervous system. Radiol Bras. 2017;50(4):IX. doi:10.1590/0100-3984.2017.50.4e3
Magnetic resonance neurography is used when one or more of the following are present 3 Lopes FCR. Neurography - a new look at the peripheral nervous system. Radiol Bras. 2017;50(4):IX. doi:10.1590/0100-3984.2017.50.4e3 :
- Inflammatory nerve problems
- Genetic nerve conditions
- Immune-mediated conditions
- Neural tumors
- Post-traumatic alterations of the nerve
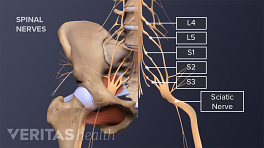
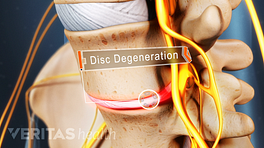
MR neurography can be used to analyze several nerve trunks at a time such as in Charcot-Marie-Tooth disease or to analyze a localized lesion, such as sciatic nerve root compression by a herniated disc. 3 Lopes FCR. Neurography - a new look at the peripheral nervous system. Radiol Bras. 2017;50(4):IX. doi:10.1590/0100-3984.2017.50.4e3
See Lumbar Herniated Disc: What You Should Know
Other imaging tests for nerve analysis include ultrasonography and computerized tomography (CT) scans.
Blood Tests
A complete blood count (CBC) can help detect blood disorders, such as anemia, infections, clotting problems, cancers, and immune-mediated disorders. A basic metabolic panel exam is used to analyze the health of bones and organs, such as the kidneys and liver. Conditions such as diabetes may be diagnosed using this test.
Other specialized blood tests may be ordered if genetic disorders or cancer is suspected.
Doctors Who Diagnose Foot Drop
Foot drop can be diagnosed by several types of physicians. If the lower back is suspected as a cause, it may be advisable to see a spine specialist, such as a physiatrist, orthopedic surgeon, or neurosurgeon. Diabetes or other metabolic conditions may be diagnosed and treated by an endocrinologist.
Once a cause is determined, various foot drop treatments may be implemented depending on the specific underlying condition.
- 1 Daniels SP, Feinberg JH, Carrino JA, Behzadi AH, Sneag DB. MRI of Foot Drop: How We Do It. Radiology. 2018;289(1):9-24. doi:10.1148/radiol.2018172634
- 2 Craig A, Richardson JK. Localized peripheral neuropathies. In: A Comprehensive Guide to Geriatric Rehabilitation. Elsevier; 2014:233-241. doi:10.1016/b978-0-7020-4588-2.00033-4
- 3 Lopes FCR. Neurography - a new look at the peripheral nervous system. Radiol Bras. 2017;50(4):IX. doi:10.1590/0100-3984.2017.50.4e3