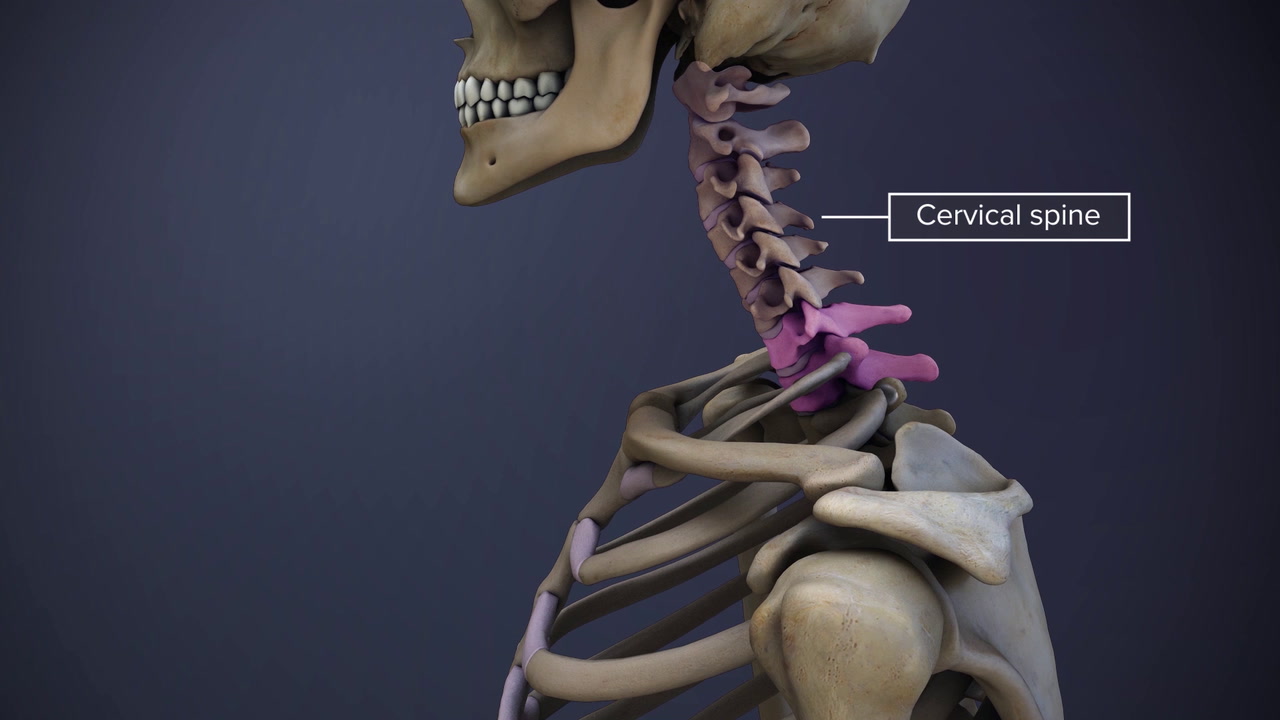
The C7-T1 spinal motion segment connects the neck (cervical spine) with the upper back (thoracic spine). Together they form the cervicothoracic junction (CTJ). Important features of this junction are:
- The highly flexible neck transitions to an almost inflexible upper back.
- The CTJ is about half as flexible as the cervical spine. 1 Simon S, Davis M, Odhner D, Udupa J, Winkelstein B. CT Imaging Techniques for Describing Motions of the Cervicothoracic Junction and Cervical Spine During Flexion, Extension, and Cervical Traction. Spine. 2006;31(1):44-50. doi:10.1097/01.brs.0000192679.25878.f9
- The lordosis or backward curvature of the cervical spine reverses into kyphosis or forward curvature of the thoracic spine.
These factors create an area of increased stress at the CTJ, both at rest and during movement. This area of stress may lead to CTJ dysfunction or instability during an injury, infection, or tumors that may affect this region. 2 Chen J, Eismont FJ. Cervicothoracic Trauma: Diagnosis and Treatment. Seminars in Spine Surgery. 2005;17(2):84-90. doi:10.1053/j.semss.2005.05.005 , 3 Wang VY, Chou D. The cervicothoracic junction. Neurosurg Clin N Am. 2007;18(2):365-71.
Anatomy of the C7-T1 Spinal Motion Segment
The C7-T1 motion segment includes the following structures:
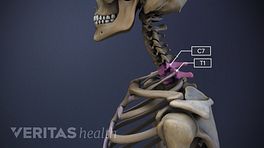
- C7 and T1 vertebrae. These vertebrae are connected by a pair of facet joints in the back and each has a vertebral body, 2 pedicles, 2 transverse processes (bony humps on the side where muscles can attach and pull on the vertebrae), 2 lamina, and a spinous process. The distinguishing features include:
- C7, also called vertebra prominens, is the last cervical vertebra. T1 is the first thoracic vertebra.
- C7 has a longer spinous process (bony protrusion), which can be felt in the back of the neck. T1’s spinous process projects at a more downward angle and may not be as prominent.
- T1 connects to the first rib with costovertebral joints. These vertebrae are held together with ligaments at multiple attachment points.
- C7-T1 intervertebral disc. A disc made of a thick fibrous ring (annulus fibrosus) that surrounds an inner gel-like material (nucleus pulposus) is situated between the C7 and T1 vertebrae. This disc protects the vertebrae by providing cushioning and shock-absorbing functions during neck movements.
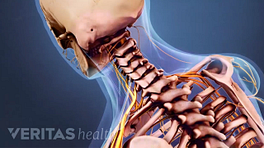
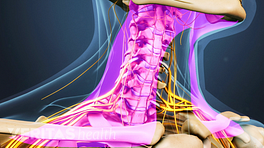
- C8 spinal nerve. The C8 spinal nerve exits the spinal cord in between the C7 and T1 vertebrae through a small bony opening called the intervertebral foramen. This nerve has a sensory root and a motor root.
- The C8 dermatome is an area of skin that receives sensation through the C8 nerve. This dermatome can vary, but it typically includes areas of skin over parts of the neck, shoulder, forearm, hand, and the little finger.
- The C8 myotome is a group of muscles controlled by the C8 nerve. These muscles commonly include those involved in bending the wrist and the fingers.
Watch Cervical Spine Anatomy Video
The vertebral bodies and arches protect the spinal cord within the spinal canal.
In This Article:
- All About the C7-T1 Spinal Segment (Cervicothoracic Junction)
- C7-T1 Treatment
- Spinal Motion Segment: C7-T1 (Cervicothoracic Junction) Animation
Potential Problems at C7-T1
While the diagnosed problems at the C7-T1 level are less common, 2 Chen J, Eismont FJ. Cervicothoracic Trauma: Diagnosis and Treatment. Seminars in Spine Surgery. 2005;17(2):84-90. doi:10.1053/j.semss.2005.05.005 research suggests that CTJ injuries may be missed during due to difficulties in visualizing this region on plain X-Ray films. 3 Wang VY, Chou D. The cervicothoracic junction. Neurosurg Clin N Am. 2007;18(2):365-71. A few conditions that may affect the CTJ are:
- Fracture. An estimated 2% to 9% of cervical spine fractures occur at the CTJ. These fractures usually include burst fractures (severely compressed or crushed vertebrae), facet joint fractures, and dislocation of the C7 and/or T1 vertebrae. Sometimes, ligament injuries may also occur.
3
Wang VY, Chou D. The cervicothoracic junction. Neurosurg Clin N Am. 2007;18(2):365-71.
,
4
Techy F, Benzel EC. Stabilization of the Cervicothoracic Junction. Contemporary Spine Surgery. 2011;12(5):1-6. doi:10.1097/01.css.0000397229.07261.72
,
5
Ohya J, Bray DP, Magill ST, Vogel TD, Berven S, Mummaneni PV. Mini-open anterior approach for cervicothoracic junction fracture: technical note. Neurosurgical Focus. 2017;43(2):E4. doi:10.3171/2017.5.focus17179
A fracture of the spinous process of C7 and/or T1 is called clay-shoveler’s fracture. This fracture occurs due to repetitive and forceful pull of the upper back muscles on these spinous processes. 6 Posthuma de boer J, Van wulfften palthe AF, Stadhouder A, Bloemers FW. The Clay Shoveler's Fracture: A Case Report and Review of the Literature. J Emerg Med. 2016;51(3):292-7. - Tumors. Tumors affecting the CTJ are usually the advanced (metastatic) type. The most common tumor that extends between the rib and the vertebra at the CTJ is the Pancoast tumor from the lung(s). Thyroid and esophageal (food pipe) tumors may also extend into the CTJ, damaging the vertebrae. The CTJ may also be affected by lesions of prostrate or breast cancer that spread to this region in advanced stages of the disease. 3 Wang VY, Chou D. The cervicothoracic junction. Neurosurg Clin N Am. 2007;18(2):365-71. , 4 Techy F, Benzel EC. Stabilization of the Cervicothoracic Junction. Contemporary Spine Surgery. 2011;12(5):1-6. doi:10.1097/01.css.0000397229.07261.72
- Infection. The CTJ may be affected by bone infections such as osteomyelitis or lung infections such as tuberculosis. 3 Wang VY, Chou D. The cervicothoracic junction. Neurosurg Clin N Am. 2007;18(2):365-71. , 4 Techy F, Benzel EC. Stabilization of the Cervicothoracic Junction. Contemporary Spine Surgery. 2011;12(5):1-6. doi:10.1097/01.css.0000397229.07261.72
- Scoliosis. Scoliosis is the sideways curvature of the spine and may occur at the CTJ due to injury, congenital birth anomaly, or unknown causes (idiopathic).
- Postsurgical instability. Laminectomies of the cervical vertebrae at or just above the CTJ may cause instability in the region. 2 Chen J, Eismont FJ. Cervicothoracic Trauma: Diagnosis and Treatment. Seminars in Spine Surgery. 2005;17(2):84-90. doi:10.1053/j.semss.2005.05.005 , 3 Wang VY, Chou D. The cervicothoracic junction. Neurosurg Clin N Am. 2007;18(2):365-71. , 4 Techy F, Benzel EC. Stabilization of the Cervicothoracic Junction. Contemporary Spine Surgery. 2011;12(5):1-6. doi:10.1097/01.css.0000397229.07261.72
In severe cases, CTJ injuries may affect the spinal cord or the C8 nerve roots. Rarely, C8 nerve injury may cause Horner’s syndrome characterized by drooping eyelids, small pupils, and sunken eyeballs usually affecting one side of the face. 7 Khan Z, Bollu PC. Horner Syndrome. [Updated 2019 Jan 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK500000/
Common Symptoms and Signs Stemming from C7-T1
A vertebral, rib, and/or disc injury at the C7-T1 level may cause moderate to severe neck pain and/or upper back pain. Sometimes, there may be difficulty in breathing if the first rib or rib muscles are injured.
If the C8 nerve is compressed or irritated, additional symptoms may occur, such as:
- Pain in parts of the shoulder, forearm, hand, and/or little finger.
- Numbness in the forearm and/or hand
- Weakness in the wrist, hand, and/or fingers.
If the spinal cord is injured, the upper and/or lower limbs and the torso may be completely or partially paralyzed. 2 Chen J, Eismont FJ. Cervicothoracic Trauma: Diagnosis and Treatment. Seminars in Spine Surgery. 2005;17(2):84-90. doi:10.1053/j.semss.2005.05.005 There may also be changes in bowel and/or bladder functions.
Nonsurgical treatments are usually tried first to treat CTJ injuries. In cases where instability of the CTJ occurs or when nonsurgical treatments do not provide relief, surgery may be considered.
- 1 Simon S, Davis M, Odhner D, Udupa J, Winkelstein B. CT Imaging Techniques for Describing Motions of the Cervicothoracic Junction and Cervical Spine During Flexion, Extension, and Cervical Traction. Spine. 2006;31(1):44-50. doi:10.1097/01.brs.0000192679.25878.f9
- 2 Chen J, Eismont FJ. Cervicothoracic Trauma: Diagnosis and Treatment. Seminars in Spine Surgery. 2005;17(2):84-90. doi:10.1053/j.semss.2005.05.005
- 3 Wang VY, Chou D. The cervicothoracic junction. Neurosurg Clin N Am. 2007;18(2):365-71.
- 4 Techy F, Benzel EC. Stabilization of the Cervicothoracic Junction. Contemporary Spine Surgery. 2011;12(5):1-6. doi:10.1097/01.css.0000397229.07261.72
- 5 Ohya J, Bray DP, Magill ST, Vogel TD, Berven S, Mummaneni PV. Mini-open anterior approach for cervicothoracic junction fracture: technical note. Neurosurgical Focus. 2017;43(2):E4. doi:10.3171/2017.5.focus17179
- 6 Posthuma de boer J, Van wulfften palthe AF, Stadhouder A, Bloemers FW. The Clay Shoveler's Fracture: A Case Report and Review of the Literature. J Emerg Med. 2016;51(3):292-7.
- 7 Khan Z, Bollu PC. Horner Syndrome. [Updated 2019 Jan 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK500000/