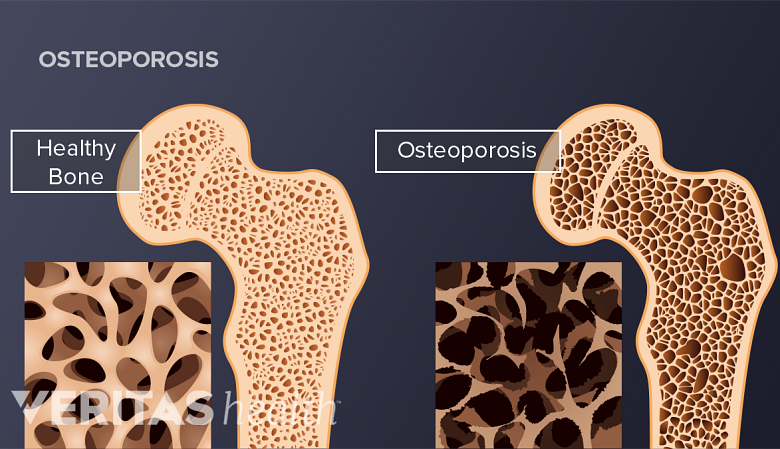
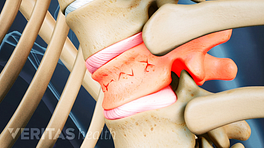
Osteoporosis is a condition of low bone density and structural deterioration of bone tissue that causes an increased risk of fractures. Osteoporosis on its own does not cause pain or obvious symptoms. Complications from the condition, including vertebral fractures, may result in back pain and limited mobility.
To catch osteoporosis early, as well as to identify those at risk of fractures caused by the condition, screening for risk factors is advised on the basis of age and sex. If screening identifies a relatively high risk for osteoporosis, a bone density test (densitometry) may be ordered.
In general, all women over age 65 and younger postmenopausal women with risk factors should be screened for low bone density. Some recommendations call for women to be screened as early as age 50. 1 Final Recommendation Statement: Osteoporosis to Prevent Fractures: Screening. U.S. Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/osteoporosis-screening1. July 2018. Accessed April 2019. While there is no official recommendation in the U.S. for men, who are less at risk, it is generally advised that men over 70 are screened. 1 Final Recommendation Statement: Osteoporosis to Prevent Fractures: Screening. U.S. Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/osteoporosis-screening1. July 2018. Accessed April 2019.
In This Article:
Bone Remodeling and Osteoporosis
Osteoporosis occurs when the bone breaks down faster than it can reform.
Bone is formed through a different process than most other tissues in the body that grow by cells dividing in two. Instead, bone undergoes a continuous process of breaking down old cells and building new cells in their place. Osteoporosis occurs when bone breaks down faster than it can reform, leading to depleted bone density.
The process of bone growth is called remodeling. Bone remodeling consists of the following:
- First, large cells called osteoclasts release enzymes that break down existing bone cells.
- Fragmented bone cells are processed (or “digested”) in the osteoclast.
- The calcium and phosphorus from the fragmented bone cells are released into the bloodstream in a process called resorption.
- Other cells called osteoblasts produce a variety of enzymes, growth factors, and hormones that create a matrix of cells in a process called bone formation.
- The osteoblasts are absorbed into the matrix and become osteocytes (bone cells).
Most people reach peak bone mass between ages 18 and 25, 2 Cosman F, de Beur SJ, LeBoff MS. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Osteoporos Int. 2014;25(10):2359–2381. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4176573/. doi:10.1007/s00198-014-2794-2. when bone remodeling and resorption occur at about the same rate. As a person ages, the hormones that influence bone remodeling and resorption tend to change and more bone is broken down than can be rebuilt. 2 Cosman F, de Beur SJ, LeBoff MS. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Osteoporos Int. 2014;25(10):2359–2381. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4176573/. doi:10.1007/s00198-014-2794-2.
Who Is Affected by Osteoporosis
Osteoporosis is one of the most common issues leading to back pain in the U.S. Roughly 500,000 spinal fractures occur due to osteoporosis every year. 3 Cannada LK, Hill BW. Osteoporotic Hip and Spine Fractures: A Current Review. Geriatr Orthop Surg Rehabil. 2014;5(4):207–212. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4252159/. Published Sept 5, 2014. Accessed April 2019.
See Osteoporosis: The Primary Cause of Collapsed Vertebrae
Because bone growth naturally slows down later in life, osteoporosis can affect both men and women over age 50. The largest population affected by osteoporosis is postmenopausal women.
See Who Is at Risk for Osteoporosis?
Transgender men and women taking hormone replacement therapy may be at increased risk of osteoporosis if they skip or stop taking hormones. 4 Ashbee O, Goldberg JM. Transgender People and Osteoporosis. Rainbow Health Ontario. Published 2006. Updated August 20, 2018. Accessed April 2019. However, very little transgender health research has been conducted to determine if transgender people in general have a higher risk for osteoporosis. 4 Ashbee O, Goldberg JM. Transgender People and Osteoporosis. Rainbow Health Ontario. Published 2006. Updated August 20, 2018. Accessed April 2019.
- 1 Final Recommendation Statement: Osteoporosis to Prevent Fractures: Screening. U.S. Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/osteoporosis-screening1. July 2018. Accessed April 2019.
- 2 Cosman F, de Beur SJ, LeBoff MS. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Osteoporos Int. 2014;25(10):2359–2381. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4176573/. doi:10.1007/s00198-014-2794-2.
- 3 Cannada LK, Hill BW. Osteoporotic Hip and Spine Fractures: A Current Review. Geriatr Orthop Surg Rehabil. 2014;5(4):207–212. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4252159/. Published Sept 5, 2014. Accessed April 2019.
- 4 Ashbee O, Goldberg JM. Transgender People and Osteoporosis. Rainbow Health Ontario. Published 2006. Updated August 20, 2018. Accessed April 2019.