Many cases of degenerative scoliosis are never diagnosed because they often do not cause symptoms. However, when degenerative scoliosis becomes painful and problematic, the symptoms and severity can vary from person to person.
In This Article:
- All About Degenerative Scoliosis
- Degenerative Scoliosis Symptoms and Diagnosis
- Treatment for Degenerative Scoliosis
- Surgery for Degenerative Scoliosis
- Degenerative Scoliosis Video
Common Degenerative Scoliosis Symptoms
Back pain from degenerative scoliosis worsens over time.
Typical signs and symptoms of degenerative scoliosis include:
- Pain comes on gradually. Back pain from degenerative scoliosis does not start suddenly. Rather, it slowly worsens over time and tends to be associated with activity. The initial pain can begin as a dull ache or stiffness, and it is usually located in the low back or less commonly in the mid back.
- Pain is worse in the morning. The pain tends to be more intense first thing in the morning, then it improves after the person gets up and starts moving around for the day. However, the pain can worsen again toward the end of the day or after vigorous or strenuous activities.
- Sitting feels better than standing/walking. The facet joints generate much of the pain, and they have more loading (pressure) in the standing position. Sitting takes the stress and weight off these joints.
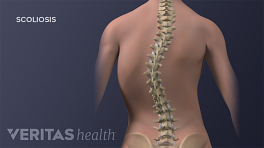
- Postural changes. Due to progressing curvature and degeneration of the spine, the shoulders and/or hips might become uneven, and a person can become shorter.
Sometimes pain might be felt in one leg but not the other. However, the direction of the scoliosis curve does not seem to correlate with which leg might feel pain. 1 De Vries AB, Mullender MG, Pluymakers WJ, Castelein RM, Van Royen BJ. Spinal decompensation in degenerative lumbar scoliosis. Eur Spine J. 2010; 19(9): 1540-4.
When Degenerative Scoliosis Symptoms Require Medical Attention
Worsening degenerative scoliosis symptoms like pain, tingling, and numbness require medical attention.
Degenerative scoliosis symptoms can worsen over time and eventually interfere with daily activities. When spinal degeneration and/or the curve progresses enough, the following could start to occur:
- Radicular symptoms. If a nerve root becomes impinged, such as by bone overgrowth or spur in the foramen (bony hole where nerve root exits the spine), radicular symptoms may occur. These symptoms can include pain, tingling, numbness, and/or weakness that radiates down the low back and into the buttock, thigh, calf, and/or foot. In some cases, radicular pain can feel searing or shock-like. Radicular symptoms are usually felt on only one side of the body.
-
Neurogenic claudication. If the lumbar spinal canal narrows, called lumbar spinal stenosis, then compressed nerves could cause the patient to experience leg pain and/or muscle cramps while walking. Typically, this type of pain will be in both legs and start after the person has walked a relatively short distance, such as a city block or two.
See Lumbar Spinal Stenosis Treatment
The pain can be relieved almost immediately by sitting down. Some patients report that flexing or bending the spine forward can also alleviate the pain, which is why some find walking uphill is less painful than walking downhill or on a flat surface. Frequently people find leaning forward on a shopping cart or walker significantly decreases their pain or increases the distance they can tolerate walking. However, severe neurogenic claudication is sometimes felt even at rest or when flexing forward.
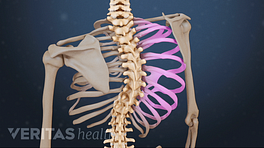
- Severe spinal deformity. A scoliosis curve that reaches 90 or 100 degrees or more could cause the patient to hunch forward (also called kyphosis), lean to the side, or both. Such a drastic change in the spine’s curvature can cause balance problems, and the spine’s abnormal rotation could also start to push the rib cage against the heart, lungs, or other internal organs.
Degenerative scoliosis rarely impinges or irritates the spinal cord (or the cauda equina nerve bundle beneath the spinal cord) enough to cause significant leg weakness or bladder/bowel control problems.
Diagnosing Degenerative Scoliosis
Finding the Cobb angle helps clinicians diagnose the severity of scoliosis.
To make an accurate diagnosis and develop an effective treatment plan, the doctor will typically follow this process:
- Take a patient history. A full medical history of the patient is collected, such as past illnesses or injuries, medications, lifestyle habits, family history, and when current problems began. This information will help the doctor to narrow down which symptoms or conditions may need further investigation.
-
Perform a physical exam. Taking into account the patient’s history, a physical exam will likely be conducted in the office to further narrow down which conditions could be the underlying cause of the patient’s symptoms. The doctor might palpate (feel) the spine as well as observe the patient in different positions.
The physical exam can check the patient’s strength, flexibility, and reflexes. If neurological symptoms, such as shock-like pain, tingling, numbness, or weakness in one or both legs are found, then an imaging study is also likely to be requested. - Request an imaging study. An MRI, CT scan, or X-ray could show degeneration of the spine. For instance, radiologic findings of narrowed disc spaces or bone spurs on vertebrae could be signs of osteoarthritis. Furthermore, an X-ray of the spine can be used to measure the Cobb angle, which is the sideways curvature of the spine. A Cobb angle of 10 degrees or more would confirm scoliosis.
See Introduction to Diagnostic Studies for Back and Neck Pain
In some cases, a person could have symptomatic degenerative scoliosis but not have imaging done if non-surgical care is already effectively managing the pain and symptoms.
- 1 De Vries AB, Mullender MG, Pluymakers WJ, Castelein RM, Van Royen BJ. Spinal decompensation in degenerative lumbar scoliosis. Eur Spine J. 2010; 19(9): 1540-4.