The goal of a vertebroplasty procedure is to stabilize the vertebral compression fracture to stop its painful movements. Vertebroplasty is considered a minimally invasive surgery because it is done through a small puncture in the skin instead of an open incision. A typical vertebroplasty procedure, described below, usually takes about 1 hour to complete.
In This Article:
Preparing for Vertebroplasty
It is common for no food or drink to be allowed less than 6 hours before the vertebroplasty procedure. For example, if the surgery is scheduled in the morning, the doctor might require that no food or drinks be consumed after midnight before the procedure. A small amount of water is typically allowed up to 2 hours before the surgery.
See Preparation Before Back Surgery
In addition, some restrictions on medications might be put in place in the days leading up to the surgery. Some medications might need to be discontinued, and others might require dosages to be adjusted. These restrictions can vary widely, depending on the patient’s personal health status.
Vertebroplasty Procedure Step-by-Step
While there can be variations in how vertebroplasty is performed, the procedure is normally done as follows:
- The patient goes to an x-ray suite or operating room and comfortably lies face down on a padded table where the procedure will be performed.
- The area of the back is sterilized where the needle will enter.
- Local anesthesia and light sedation are administered. Pain should not be felt in the area where the procedure takes place, but the patient typically remains awake and responsive throughout.
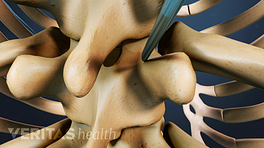
- Using contrast-enhanced fluoroscopy, which displays x-ray images on a video monitor in real-time, a bone biopsy needle is guided into the fractured vertebra through a small puncture in the skin. The fluoroscopy is necessary for positioning the needle inside the vertebral compression fracture without damaging a nearby critical structure, such as the spinal cord.
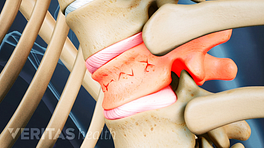
- PMMA, a specially formulated bone cement, is injected under pressure directly into the fractured vertebra. The bone cement fills the cracks within the bone to create a type of internal cast to stabilize the vertebral bone.
- The needle is removed and the cement hardens quickly (in about 10 minutes), congealing the fragments of the fractured vertebra and stabilizing the bone.
- The small skin puncture is covered with a bandage.
- The patient is typically kept under observation for a couple hours to ensure that the medications have worn off and the bone cement has hardened without causing complications. Some surgeons might require that the patient remain recumbent (lying down) for an hour or two before being allowed to slowly walk around.
After the post-procedure observation period is complete, the patient is free to leave the medical facility and can go home the same day. Patients are usually advised not to drive themselves home the day of the procedure, so a friend or family member may need to provide a ride. If the patient needs further observation after the procedure, is particularly frail, or will not have assistance at home, a short stay in the hospital may be recommended.
Recovery from Vertebroplasty
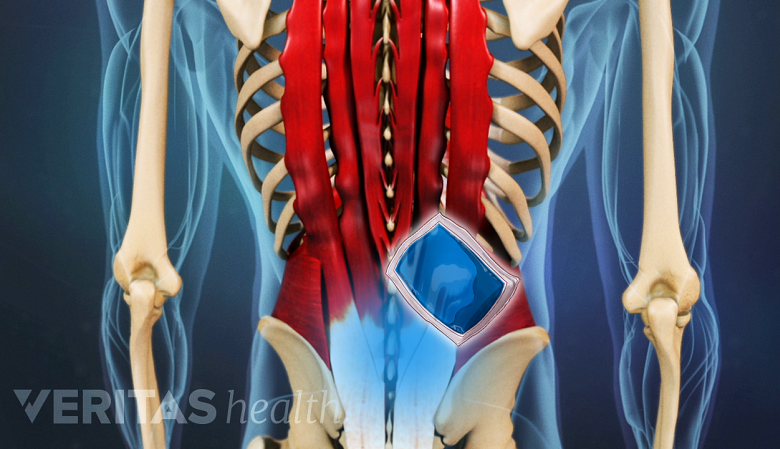
Post-surgery, brief soreness at the puncture site can be relieved with an ice pack.
For the first 24 hours after vertebroplasty, bedrest or taking it easy at home is usually recommended. Activity levels may be increased gradually and most regular medications can be resumed. There may be some soreness for a few days at the puncture site that may be relieved with an ice pack.
See Practical Advice for Recovering from Back Surgery
Most patients experience pain relief within 24 to 48 hours after surgery. A return to more strenuous physical activities, such as participating in sports or heavy lifting, might not be advised for up to 6 weeks.
A follow-up appointment with the doctor is typically scheduled a couple weeks after surgery to ensure that the recovery is going well.