Tramadol is commonly prescribed to treat back pain, however, it should be taken with caution. Some of the major considerations when taking tramadol include:
- Side effects
- Interactions with other medications
- Possible health risks
- Withdrawal symptoms
Some restrictions on life and work may be required due to tramadol’s effect on the body. Driving, operating machinery, and other activities requiring mental and physical coordination may be unsafe.
See Medications for Back Pain and Neck Pain
Tramadol may not be as safe as NSAIDs in the use of osteoarthritis-related pain. For patients over age 50, mortality is higher for those using tramadol as opposed to using NSAIDs like naproxen, diclofenac, or celecoxib.
In This Article:
- Tramadol for Back Pain
- Tramadol: Potential Side Effects, Interactions, Risks, and Complications
- Medications for Back Pain Video
Side Effects of Tramadol
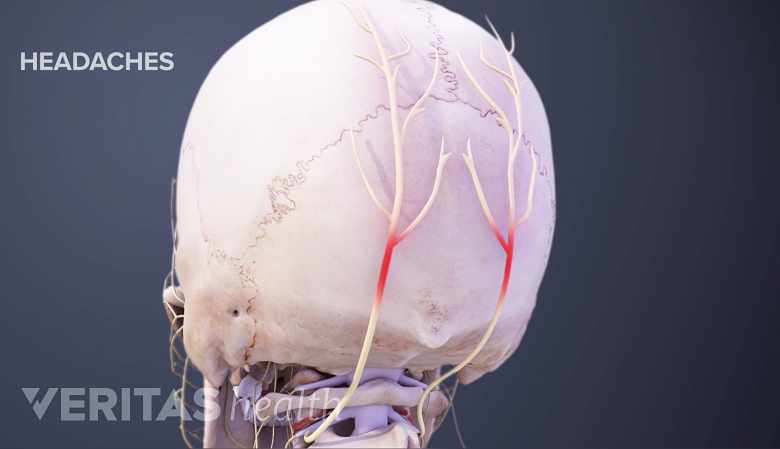
Headaches are a potential side effect of pain medications like tramadol.
As with most medications tramadol may have side effects. Common side effects include:
- Headache
- Dizziness
- Drowsiness or sleepiness
- Constipation
- Dry mouth
These side effects are typically mild and may go away within a few days or weeks. Seek medical attention if they increase or do not go way.
Potential Interactions and Complications
Certain conditions could increase the risks of complications. Patients are encouraged to answer their health care provider’s questions honestly and notify them of the following:
- Any current or past drug or alcohol abuse
- History of depression
- Past head injuries
- Epilepsy or history of seizures
- Liver or kidney problems
The health care provider should also be informed if the person is pregnant or breastfeeding. People who are suicidal or prone to addiction should not take tramadol.
Drug interactions
Keeping the prescriber and pharmacist informed about all other medications and supplements being taken is crucial when taking tramadol. Drug and supplement interactions with tramadol can be life-threatening. Combining tramadol with alcohol, sedatives, or other opioid medications can also lead to serious medical complications, including overdose.
Older adults tend to process medications differently and should be especially cautious when taking tramadol.
Possible Health Risks Associated with Tramadol
Tramadol is associated with a number of risks that can be life threatening if not treated appropriately.
- Seizures. Seizures are among the most serious potential problems associated with tramadol. While a seizure can occur while taking the recommended dose, seizures are more likely in those who have taken high doses of tramadol or combined tramadol with other medications. Additionally, other factors that can increase the risk of seizure include, but are not limited to:
- Those who have epilepsy
- People with a history of seizures
- Individuals with a recognized risk for seizure (such as head trauma, metabolic disorders, alcohol and drug withdrawal, and central nervous system infections)
- People taking selective-serotonin reuptake inhibitor and serotonin-norepinephrine reuptake inhibitors (SNRIs)
- Those taking antidepressants or appetite suppressants
- People taking tricyclic compounds, such as cyclobenzaprine, promethazine, and tricyclic antidepressants (TCAs)
- Individuals taking other opioids
- Serotonin syndrome. This condition is classified as a group of symptoms that occur when the body’s levels of serotonin are increased. The syndrome can be fatal, but often the symptoms go away when the medication is stopped. Symptoms include shivering, muscle stiffness, confusion, and a high fever. Signs of serotonin syndrome should prompt an immediate call to the doctor or a visit to the emergency room.
- Breathing problems. Although the risk is less with tramadol than with other opioids, such as morphine, some people who take the medication may develop a breathing problem. This problem, called respiratory depression, causes breathing to become slow and shallow. Individuals with asthma or other lung problems may be advised to avoid tramadol. Dangerous breathing problems are more likely when drinking alcohol or taking other drugs—legal or illegal—while using tramadol. Respiratory depression is more common in older adults and those in poor overall health.
- Potential for dependence and addiction. Tramadol is classified as a controlled substance that has a risk of misuse. It is a Schedule IV drug, a category that includes Xanax, Valium, and Ambien.
See The Difference Between Opioid Addiction and Physical Dependence
A person may not experience all or any of these risks.
Withdrawal symptoms
Patients should not stop taking tramadol suddenly. Discontinuing tramadol use should be done gradually and under the guidance of a physician who can develop an individualized tapering schedule to minimize withdrawal symptoms.
See Opioid Detoxification and Withdrawal
Stopping the medication all at once may produce unpleasant, and even dangerous, withdrawal symptoms, such as nervousness, chills, nausea, and diarrhea. Additionally, the FDA has reported instances of uncontrolled pain, psychological distress, and suicide as a result of discontinuation or rapidly decreasing the dose of opioid pain medications. 1 FDA Drug Safety Commission website, FDA identifies harm reported from sudden discontinuation of opioid pain medicines and requires label changes to guide prescribers on gradual, individualized tapering. April 9, 2019. https://www.fda.gov/drugs/drug-safety-and-availability/fda-identifies-harm-reported-sudden-discontinuation-opioid-pain-medicines-and-requires-label-changes
Tramadol is considered to have fewer potential risks and complications when compared to other strong pain medications. It is often prescribed for patients who have had adverse reactions to other pain medications. However, serious side effects and risks still exist.
- 1 FDA Drug Safety Commission website, FDA identifies harm reported from sudden discontinuation of opioid pain medicines and requires label changes to guide prescribers on gradual, individualized tapering. April 9, 2019. https://www.fda.gov/drugs/drug-safety-and-availability/fda-identifies-harm-reported-sudden-discontinuation-opioid-pain-medicines-and-requires-label-changes