The addition of multiple levels in a spinal fusion surgery increases the complexity of the procedure and may also increase the risk of adverse events or complications compared to single-level fusion surgery. 1 Stanton EW, Chang KE, Formanek B, Buser Z, Wang J. The incidence of failed back surgery syndrome varies between clinical setting and procedure type. J Clin Neurosci. 2022 Sep;103:56-61. doi: 10.1016/j.jocn.2022.06.027
In This Article:
Immediate surgical risks
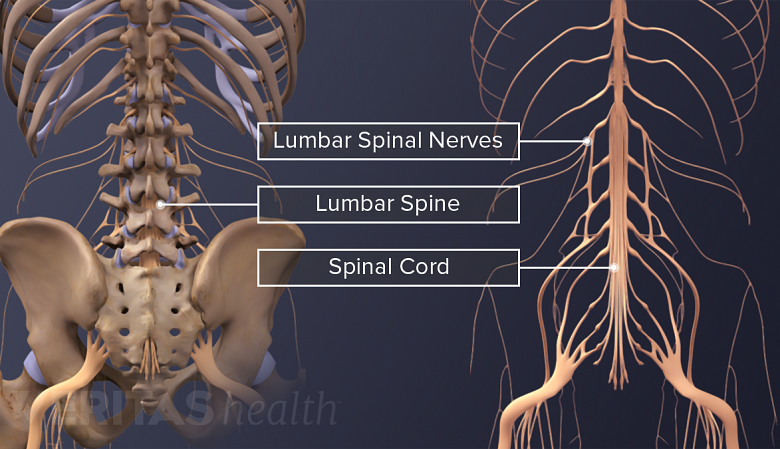
Lumbar fusion surgery can result in serious neurological problems like cauda equina syndrome and nerve injuries.
Immediate surgical risks include adverse events, which typically occur immediately after the surgery but may also occur over time. Research indicates that around 24% to 35% of patients may need revision surgery due to an adverse event or complication. 2 Röllinghoff M, Schlüter-Brust K, Groos D, et al. Mid-range outcomes in 64 consecutive cases of multilevel fusion for degenerative diseases of the lumbar spine. Orthop Rev (Pavia). 2010;2(1):e3. doi:10.4081/or.2010.e3 , 3 Ibrahim JM, Singh P, Beckerman D, et al. Outcomes and Quality of Life Improvement After Multilevel Spinal Fusion in Elderly Patients. Global Spine J. 2020;10(2):153-159. doi:10.1177/2192568219849393
- Multilevel procedures take longer than single-level fusions, and potential problems with blood loss, blood clotting, and post-surgical wound infections are directly related to the length of surgery. 4 Hu SS. Blood loss in adult spinal surgery. Eur Spine J. 2004;13 Suppl 1(Suppl 1):S3-S5. doi:10.1007/s00586-004-0753-x , 5 Mahesh B, Upendra B, Vijay S, Kumar GA, Reddy S. Complication rate during multilevel lumbar fusion in patients above 60 years. Indian J Orthop. 2017;51(2):139-146. doi:10.4103/0019-5413.201704 The risk of blood loss also increases with obesity, advanced age, and the number of fused levels. 5 Mahesh B, Upendra B, Vijay S, Kumar GA, Reddy S. Complication rate during multilevel lumbar fusion in patients above 60 years. Indian J Orthop. 2017;51(2):139-146. doi:10.4103/0019-5413.201704 , 6 Schoell K, Wang C, D’Oro A, et al. Depression increases the rates of neurological complications and failed back surgery syndrome in patients undergoing lumbar spine surgery. Clinical Spine Surgery: A Spine Publication. 2019;32(2):E78-E85. doi:10.1097/BSD.0000000000000730
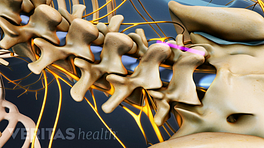
- The potential for nerve and spinal cord damage is a concern with any type of spinal surgery. Fusion surgeries approached from the back, such as posterior lumbar interbody fusion (PLIF), have a higher rate of neurological damage compared to surgeries approached from the front, such as anterior lumbar interbody fusion (ALIF). 6 Schoell K, Wang C, D’Oro A, et al. Depression increases the rates of neurological complications and failed back surgery syndrome in patients undergoing lumbar spine surgery. Clinical Spine Surgery: A Spine Publication. 2019;32(2):E78-E85. doi:10.1097/BSD.0000000000000730
- Serious neurologic conditions, such as cauda equina syndrome and injury to the spinal nerves, are the reported neurological complications of lumbar fusion surgeries. The risk of neurological complications increases with advanced age and is typically higher in women. 6 Schoell K, Wang C, D’Oro A, et al. Depression increases the rates of neurological complications and failed back surgery syndrome in patients undergoing lumbar spine surgery. Clinical Spine Surgery: A Spine Publication. 2019;32(2):E78-E85. doi:10.1097/BSD.0000000000000730 Tear of the dural membrane, which surrounds the spinal nerves and holds the spinal fluid, is also fairly common with multilevel fusion surgeries including decompression. This condition is called durotomy and occurs in up to 20% of spine fusion and/or decompression surgeries. 7 Alluri R, Kang HP, Bouz G, Wang J, Hah RJ. The true effect of a lumbar dural tear on complications and cost. Spine. 2020;45(3):E155-E162. doi:10.1097/BRS.0000000000003213
In general, factors such as advanced age (over 70 years), underlying health conditions, and pre-existing problems in the spinal discs or joints with prior surgery increase the likelihood of developing complications after multilevel fusion surgery. 2 Röllinghoff M, Schlüter-Brust K, Groos D, et al. Mid-range outcomes in 64 consecutive cases of multilevel fusion for degenerative diseases of the lumbar spine. Orthop Rev (Pavia). 2010;2(1):e3. doi:10.4081/or.2010.e3 , 3 Ibrahim JM, Singh P, Beckerman D, et al. Outcomes and Quality of Life Improvement After Multilevel Spinal Fusion in Elderly Patients. Global Spine J. 2020;10(2):153-159. doi:10.1177/2192568219849393
Late surgical risks
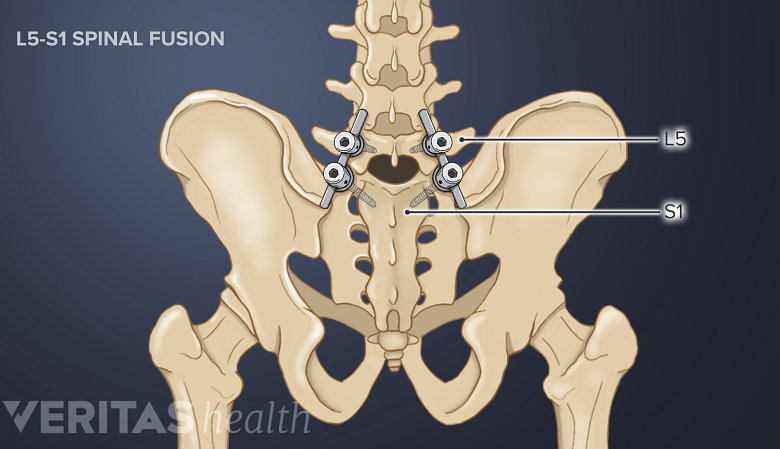
The L5-S1 spinal segment tends to experience higher rates of fusion failure.
Potential risks and complications that may arise over time as healing takes place include:
- Loss of adjacent stability. It is common for surgeons to decompress a spinal level above or below a fused segment.
8
Smorgick Y, Park DK, Baker KC, et al. Single- versus multilevel fusion for single-level degenerative spondylolisthesis and multilevel lumbar stenosis: four-year results of the spine patient outcomes research trial. Spine (Phila Pa 1976). 2013;38(10):797-805. doi:10.1097/BRS.0b013e31827db30f
Decompression is a surgical procedure that is performed to alleviate pain caused by pinched spinal nerves. During a lumbar decompression back surgery, a small portion of the bone over the nerve root and/or disc material from under the nerve root is removed to give the nerve root more space and provide a better healing environment.
When decompression is performed above a fused segment, the integrity of the strong spinal ligaments, which act as tough bands to support and stabilize the spine (especially while bending forward), can be compromised due to excision, eventually leading to segmental instability in the region. 8 Smorgick Y, Park DK, Baker KC, et al. Single- versus multilevel fusion for single-level degenerative spondylolisthesis and multilevel lumbar stenosis: four-year results of the spine patient outcomes research trial. Spine (Phila Pa 1976). 2013;38(10):797-805. doi:10.1097/BRS.0b013e31827db30f - Fusion failure. Multilevel fusions containing 3 or more levels have a significantly higher risk of developing pseudoarthrosis (failure to achieve proper bony fusion). Failed fusions also result in loss of function and increased usage of pain medication.
9
Patel VV, Billys J, Okonkwo DO, He DY, Ryaby JT, Radcliff K. Three- and 4-level lumbar arthrodesis using adjunctive pulsed electromagnetic field stimulation: a multicenter retrospective evaluation of fusion rates and a review of the literature. Int J Spine Surg. 2021;15(2):228-233. doi:10.14444/8031
Fusion failure is typically more common in the L5-S1 spinal segment,
10
Tannoury C, Bhale R, Vora M, Saade A, Kortbawi R, Orlando G, Das A, Tannoury T. Pseudarthrosis Following Lumbar and Lumbosacral Fusion Using the Antepsoas Technique. Spine (Phila Pa 1976). 2021 Dec 15;46(24):1690-1695. doi: 10.1097/BRS.0000000000004115
occurring in up to 24% of multilevel surgeries that involve this segment.
11
Lebl DR, Sama AA, Pumberger M, Kotwal S, Cammisa FP, Girardi FP. Reamed transacral interbody fusion for l5–s1 pseudoarthrosis. Journal of Spinal Disorders & Techniques. 2013;26(6):334-341. doi:10.1097/BSD.0b013e318246b767
Specific factors that contribute to pseudoarthrosis include diabetes, obesity, osteoporosis, tobacco use, and advanced age. 9 Patel VV, Billys J, Okonkwo DO, He DY, Ryaby JT, Radcliff K. Three- and 4-level lumbar arthrodesis using adjunctive pulsed electromagnetic field stimulation: a multicenter retrospective evaluation of fusion rates and a review of the literature. Int J Spine Surg. 2021;15(2):228-233. doi:10.14444/8031 -
Implant failure. Implant failure (loosening or breakage of the screw or rod) may be associated with fusion failure and a poor clinical outcome. In the lower back, common implant-related problems include pedicle screw loosening, especially of the screws at S1, and infection. Some patients with pedicle screw loosening may develop back pain and need revision surgery to fix/remove the hardware. 2 Röllinghoff M, Schlüter-Brust K, Groos D, et al. Mid-range outcomes in 64 consecutive cases of multilevel fusion for degenerative diseases of the lumbar spine. Orthop Rev (Pavia). 2010;2(1):e3. doi:10.4081/or.2010.e3
- Adjacent segment disease. Mobile spinal levels surrounding the fused segments bear additional stresses as motion is restricted across the fusion. This additional stress is felt to contribute to a higher incidence of degeneration of adjacent segments, which could result in symptoms and the need for additional surgery in the future. This condition is known as adjacent segment disease. The stress seen by an adjacent level and the risk of adjacent segment disease is felt to be progressively higher with more levels stiffened by fusion. Therefore, it is thought that multilevel spinal fusions may have a higher risk of adjacent segment disease than single-level fusions. 2 Röllinghoff M, Schlüter-Brust K, Groos D, et al. Mid-range outcomes in 64 consecutive cases of multilevel fusion for degenerative diseases of the lumbar spine. Orthop Rev (Pavia). 2010;2(1):e3. doi:10.4081/or.2010.e3
Specific factors that contribute to adjacent segment disease include advanced age, obesity, pre-existing degeneration of the discs of the adjacent segment, and menopause. Research indicates that at least 30% of patients with lumbar spinal fusion may develop adjacent segment disease over time. 2 Röllinghoff M, Schlüter-Brust K, Groos D, et al. Mid-range outcomes in 64 consecutive cases of multilevel fusion for degenerative diseases of the lumbar spine. Orthop Rev (Pavia). 2010;2(1):e3. doi:10.4081/or.2010.e3
These complications ultimately result in failed back surgery syndrome—a generalized term that is used to describe the situation when the outcome of back surgery does not correspond with the expected results of the surgeon and the patient.
It is advisable for patients to talk to their surgeons in detail and understand the type of spine surgery, including its potential benefits, risks, and surgical alternatives before scheduling the procedure. Taking necessary precautions and following activity restrictions as instructed during the recovery period can help heal the surgical site and prevent future complications.
- 1 Stanton EW, Chang KE, Formanek B, Buser Z, Wang J. The incidence of failed back surgery syndrome varies between clinical setting and procedure type. J Clin Neurosci. 2022 Sep;103:56-61. doi: 10.1016/j.jocn.2022.06.027
- 2 Röllinghoff M, Schlüter-Brust K, Groos D, et al. Mid-range outcomes in 64 consecutive cases of multilevel fusion for degenerative diseases of the lumbar spine. Orthop Rev (Pavia). 2010;2(1):e3. doi:10.4081/or.2010.e3
- 3 Ibrahim JM, Singh P, Beckerman D, et al. Outcomes and Quality of Life Improvement After Multilevel Spinal Fusion in Elderly Patients. Global Spine J. 2020;10(2):153-159. doi:10.1177/2192568219849393
- 4 Hu SS. Blood loss in adult spinal surgery. Eur Spine J. 2004;13 Suppl 1(Suppl 1):S3-S5. doi:10.1007/s00586-004-0753-x
- 5 Mahesh B, Upendra B, Vijay S, Kumar GA, Reddy S. Complication rate during multilevel lumbar fusion in patients above 60 years. Indian J Orthop. 2017;51(2):139-146. doi:10.4103/0019-5413.201704
- 6 Schoell K, Wang C, D’Oro A, et al. Depression increases the rates of neurological complications and failed back surgery syndrome in patients undergoing lumbar spine surgery. Clinical Spine Surgery: A Spine Publication. 2019;32(2):E78-E85. doi:10.1097/BSD.0000000000000730
- 7 Alluri R, Kang HP, Bouz G, Wang J, Hah RJ. The true effect of a lumbar dural tear on complications and cost. Spine. 2020;45(3):E155-E162. doi:10.1097/BRS.0000000000003213
- 8 Smorgick Y, Park DK, Baker KC, et al. Single- versus multilevel fusion for single-level degenerative spondylolisthesis and multilevel lumbar stenosis: four-year results of the spine patient outcomes research trial. Spine (Phila Pa 1976). 2013;38(10):797-805. doi:10.1097/BRS.0b013e31827db30f
- 9 Patel VV, Billys J, Okonkwo DO, He DY, Ryaby JT, Radcliff K. Three- and 4-level lumbar arthrodesis using adjunctive pulsed electromagnetic field stimulation: a multicenter retrospective evaluation of fusion rates and a review of the literature. Int J Spine Surg. 2021;15(2):228-233. doi:10.14444/8031
- 10 Tannoury C, Bhale R, Vora M, Saade A, Kortbawi R, Orlando G, Das A, Tannoury T. Pseudarthrosis Following Lumbar and Lumbosacral Fusion Using the Antepsoas Technique. Spine (Phila Pa 1976). 2021 Dec 15;46(24):1690-1695. doi: 10.1097/BRS.0000000000004115
- 11 Lebl DR, Sama AA, Pumberger M, Kotwal S, Cammisa FP, Girardi FP. Reamed transacral interbody fusion for l5–s1 pseudoarthrosis. Journal of Spinal Disorders & Techniques. 2013;26(6):334-341. doi:10.1097/BSD.0b013e318246b767