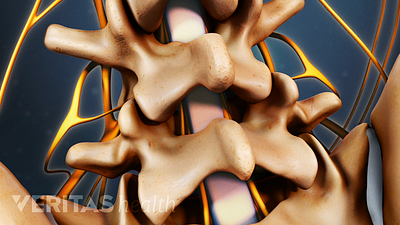
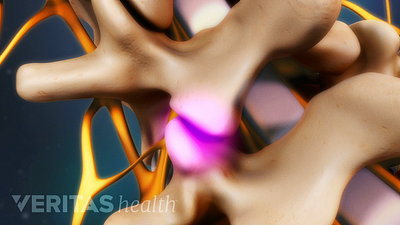
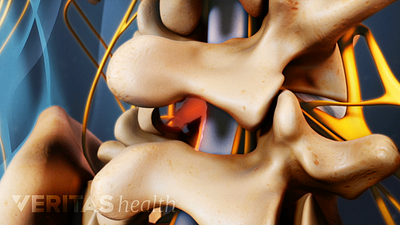
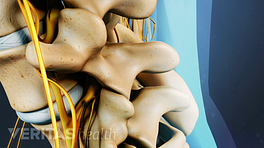
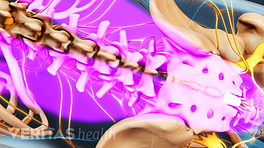
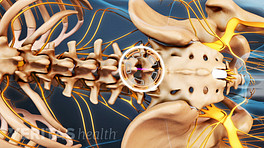
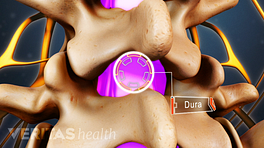
So we get questions a lot about microdiscectomy and what’s going to happen with a microdiscectomy. There’s several different techniques, some are mini-micro, some are mini-micro-nanosurgeries. And different surgeons may have different techniques to achieve the same goal. In this day and age, most surgeons consider a discectomy or microdiscectomy to be pretty much similar, that you go through a very small incision, sometimes you go through an operating tube and you use microscopic enhancement, either wearing goggles or using a microscope. And then high-intensity light so you can see down these holes as well or better than you could before when you had big open surgeries. And then they isolate where the herniated disc is And then they isolate where the herniated disc is between the nerve roots and they incise. Normally there is a thin little tissue over the herniated disc. And then once they’ve incised through that, they are able to remove that portion of the disc that has protruded out, is deviating the nerve root, elevating the nerve root, inflaming the nerve root. And that particular piece of tissue normally wants to come out. The disc has already expelled it to some degree. It has pushed it all the way out through the outer annulus, which is if we think in terms of tires is the difference between the tube inside of the tire and the rubber of the tire itself. The inner tube has ruptured out through the tough outer lining of the tire, and that’s almost exactly what we’re dealing with with a herniated disc. So we just take that fragment out, we make sure there aren’t any other loose fragments. We also make sure that in the area there are no other impingement on the nerve root, which we can resect with instruments, and then we close back up and that area heals shut.
And the pressure is off immediately. Numbness may take days or weeks or months to go away, depending upon how long it’s been there before. Pain can go away, can come back again as the nerve continues to heal if there was significant damage to the nerve root.
The doctor, most of the time it doesn’t relate, the clinical outcome, with what the nerve looks like when we’re done there. It can look perfect and in a small percentage of cases, we can continue to have leg pain. It can look terrible and smashed up when we take out the herniated disc to free up the area and the nerve root still looks bad but at least there’s nothing pushing on it; patient wakes up and they’re perfect. So your doctor is not going to be able to tell you very much from what he saw, as far as your prognosis is concerned.
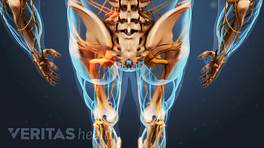
In determining why to have a microdiscectomy, it’s going to be most successful in those patients that have what we call radicular pain or leg pain. And that’s pain that radiates from the buttocks or hip down below the knee, usually into the lower leg and even more frequently into some portion of the foot. And under those circumstances, you should have a very good response from a discectomy.
If your primary complaint is back pain as well as some leg pain, you might find with the microdiscectomy that your leg gets better, but your back may not necessarily get that much better. Sometimes it does, sometimes it doesn’t. Sometimes additional testing before surgery is what you need to have done to distinguish between where the pain is coming from that’s causing your back discomfort and what’s causing your leg discomfort. Epidural steroid blocks or selective nerve root blocks, things like this sometimes can help differentiate that as a prognosticating test before you actually go to surgery.