Does your back, arm, or leg pain seem to come and go, depending on what you're doing at the moment? This sign may indicate spinal stenosis.
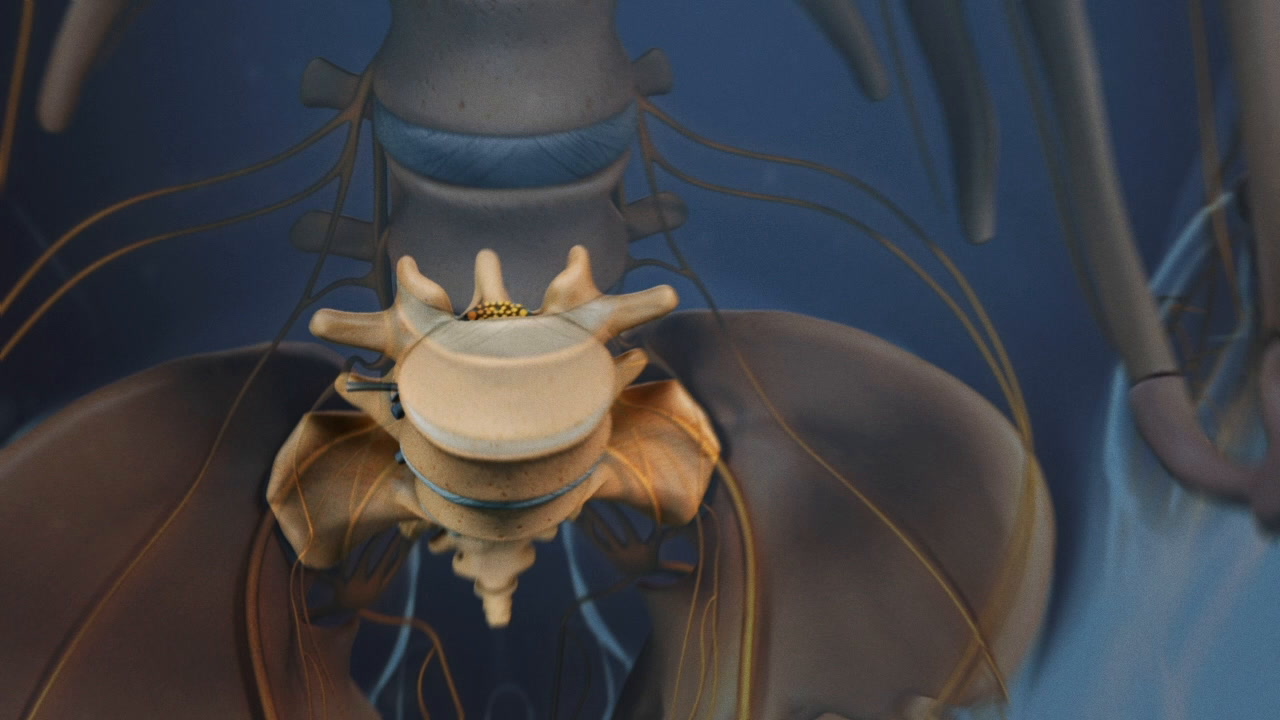
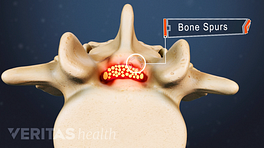
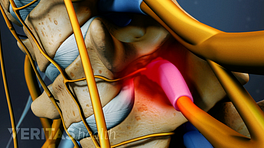
Spinal stenosis happens when the bony openings for your spinal nerves (foramen) and/or the spinal cord (central canal) become narrow. This narrowing may compress your spinal cord and/or spinal nerves and can develop at various points along your spine. Spinal stenosis is a condition that's more likely to occur in people over 60 years of age and tends to worsen as the years add up. 1 Melancia JL, Francisco AF, Antunes JL. Spinal stenosis. In: Handbook of Clinical Neurology. Elsevier; 2014:541-549. doi:10.1016/b978-0-7020-4086-3.00035-7
Here are 6 typical signs and symptoms to watch out for if you suspect your pain is from spinal stenosis. Depending on the type and location of the stenosis, one or more symptoms may be experienced:
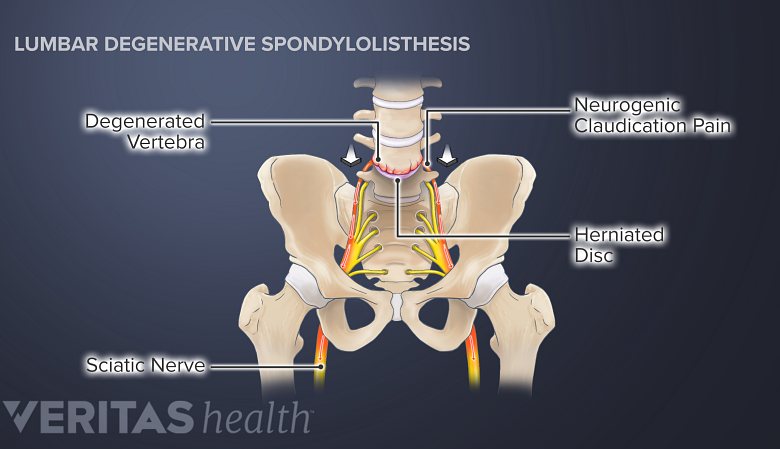
1. Neurogenic claudication
Stenosis from spinal degeneration can cause neurogenic claudication in both legs.
When the nerves in your lower back get compressed, you may experience neurogenic claudication in your legs. Neurogenic claudication usually has the following characteristics 2 Munakomi S, Foris LA, Varacallo M. Spinal Stenosis And Neurogenic Claudication. Updated Dec. 6, 2019. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430872/ :
- Constant pain and/or numbness in your legs while standing
- Increased pain and/or numbness in your legs while walking variable distances and/or while bending the spine backward
- Difficulty in performing upright exercises or activities
- Improvement or resolution of pain and/or numbness with rest
Neurogenic claudication pain is typically relieved when you bend your spine forward (such as while leaning on a shopping cart/walker, squatting, or sitting and leaning forward). 2 Munakomi S, Foris LA, Varacallo M. Spinal Stenosis And Neurogenic Claudication. Updated Dec. 6, 2019. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430872/
Your doctor will likely need to differentiate this pain from vascular claudication, which can mimic neurogenic claudication.
2. Sciatica
Compression of the nerve roots in your lower back may lead to lumbar radiculopathy or sciatica (depending on the nerve roots affected). Sciatica is experienced as nerve pain and weakness typically felt in one leg at a time.
Depending on the nerve root(s) affected, pain may occur in your lower back, buttock, thigh, calf, leg, and/or foot. A pins-and-needles sensation, tingling, weakness, and/or numbness may also occur in the areas affected by pain.
3. Foot drop
Compression of the L4 and L5 nerve roots in the lower spine may cause motor weakness in your foot, resulting in foot drop. 3 Liu K, Zhu W, Shi J, et al. Foot drop caused by lumbar degenerative disease: clinical features, prognostic factors of surgical outcome and clinical stage. PLoS One. 2013;8(11):e80375. Published 2013 Nov 5. doi:10.1371/journal.pone.0080375 This condition typically causes a feeling of weakness while attempting to lift the foot and/or toes upward. As a result, the individual may involuntarily drag their foot or tend to trip while attempting to walk. 4 Bouche P. Compression and entrapment neuropathies. In: Handbook of Clinical Neurology. Elsevier; 2013:311-366. doi:10.1016/b978-0-444-52902-2.00019-9 , 5 Larson RD, Cantrell GS, Farrell JW, Lantis DJ, Pribble BA. Assessment, Consequence, and Clinical Implication of Asymmetry. In: Nutrition and Lifestyle in Neurological Autoimmune Diseases. Elsevier; 2017:127-134. doi:10.1016/b978-0-12-805298-3.00013-x
The compression of the S1 nerve root may cause weakness while walking on tip-toes.
See Common Causes of Foot Drop
4. Gait problems
Spinal stenosis can affect walking in different ways depending on its location within the spine, for example:
- Lumbar spinal stenosis (in the lower back) may cause gait problems due to foot drop. The condition may also cause weakness in thigh and leg muscles, such as the quadriceps and the calves.
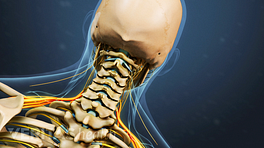
- Cervical spinal stenosis (in the neck) with spinal cord compression may cause difficulty in maintaining balance while walking, especially in the dark. 6 Meyer F, Börm W, Thomé C. Degenerative cervical spinal stenosis: current strategies in diagnosis and treatment. Dtsch Arztebl Int. 2008;105(20):366–372. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2696878/ However, cervical spine stenosis with a pinched nerve does not cause gait imbalance.
Changes in gait may be too subtle to notice at first. Over time, the condition may present with progressively increasing falls.
See Foot Drop Symptoms, Steppage Gait & Other Warning Signs
5. Radiating arm pain
Cervical spinal stenosis may cause mild to moderate burning or shock-like pain in the neck, shoulder, and/or arms. Abnormal sensations, such as tingling, crawling, and/or numbness may be felt in both hands. 6 Meyer F, Börm W, Thomé C. Degenerative cervical spinal stenosis: current strategies in diagnosis and treatment. Dtsch Arztebl Int. 2008;105(20):366–372. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2696878/ The arms and hands may feel weak.
Read more about Cervical Radiculopathy Symptoms
6. Loss of fine motor skills
Spinal stenosis in the cervical spine may cause difficulty in doing tasks that involve fine motor skills of the hand, such as buttoning a shirt. In the advanced stages, there may be difficulty with writing, eventually making holding a pen impossible. 6 Meyer F, Börm W, Thomé C. Degenerative cervical spinal stenosis: current strategies in diagnosis and treatment. Dtsch Arztebl Int. 2008;105(20):366–372. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2696878/
If these symptoms sound familiar, check with your doctor, since spinal stenosis may get worse without treatment.
Red-flag signs and symptoms of spinal stenosis
Rarely, severe spinal stenosis may cause red-flag symptoms, such as bowel and/or bladder incontinence, numbness in the inner thighs and genital area, and/or severe weakness in both legs.
These symptoms indicate a serious medical condition, such as cauda equina syndrome, which must be treated urgently to prevent permanent loss of function in the legs.
Spinal stenosis treatment options
An accurate diagnosis by a medical professional is necessary to determine the underlying cause of spinal stenosis. Depending on the cause and severity, your doctor may suggest nonsurgical treatments, such as physical therapy, pain-relieving medications, and/or activity modification. Sometimes, minimally invasive procedures, such as epidural steroid injections may be advised. Surgery is rarely advocated as the first-line treatment unless there are severe symptoms or neurologic deficits.
Learn more:
- 1 Melancia JL, Francisco AF, Antunes JL. Spinal stenosis. In: Handbook of Clinical Neurology. Elsevier; 2014:541-549. doi:10.1016/b978-0-7020-4086-3.00035-7
- 2 Munakomi S, Foris LA, Varacallo M. Spinal Stenosis And Neurogenic Claudication. Updated Dec. 6, 2019. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430872/
- 3 Liu K, Zhu W, Shi J, et al. Foot drop caused by lumbar degenerative disease: clinical features, prognostic factors of surgical outcome and clinical stage. PLoS One. 2013;8(11):e80375. Published 2013 Nov 5. doi:10.1371/journal.pone.0080375
- 4 Bouche P. Compression and entrapment neuropathies. In: Handbook of Clinical Neurology. Elsevier; 2013:311-366. doi:10.1016/b978-0-444-52902-2.00019-9
- 5 Larson RD, Cantrell GS, Farrell JW, Lantis DJ, Pribble BA. Assessment, Consequence, and Clinical Implication of Asymmetry. In: Nutrition and Lifestyle in Neurological Autoimmune Diseases. Elsevier; 2017:127-134. doi:10.1016/b978-0-12-805298-3.00013-x
- 6 Meyer F, Börm W, Thomé C. Degenerative cervical spinal stenosis: current strategies in diagnosis and treatment. Dtsch Arztebl Int. 2008;105(20):366–372. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2696878/