Studies continue to show that kyphoplasty is a relatively safe surgery for helping to restore vertebral height, correct kyphosis deformity, and eliminate pain caused by compression fractures. The overall risk for kyphoplasty-related complications is estimated to be less than 4%. 1 Wong C, McGirt MJ. Vertebral compression fractures: a review of current management and multimodal therapy. J Multidiscip Healthc. 2013; 6: 205-14. Even though complications are rare, they can potentially be serious and must be considered before agreeing to have kyphoplasty.
In This Article:
- Kyphoplasty for Vertebral Compression Fractures
- Kyphoplasty Procedure Overview
- Kyphoplasty Risks and Potential Complications
- Kyphoplasty (Osteoporosis Fracture Treatment) Video
Potential Complications of Kyphoplasty
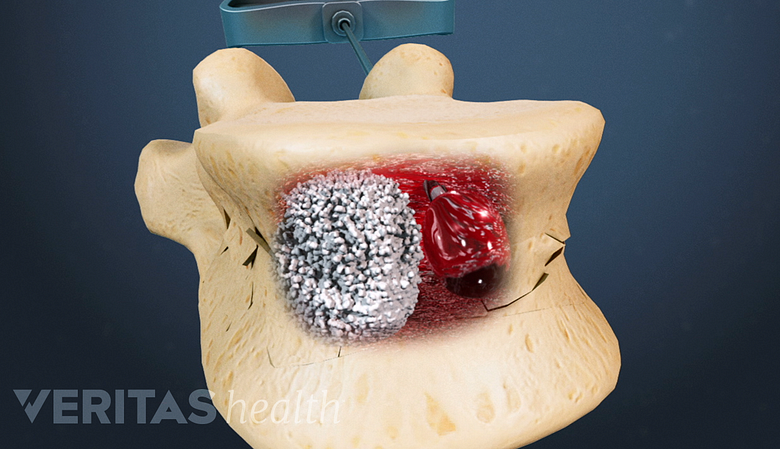
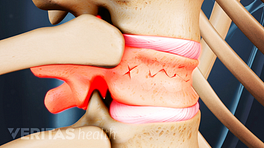
In rare cases, the bone cement might seep near the nerve root, leading to increased pain symptoms.
Some general surgical risks apply to kyphoplasty, including infection, excessive bleeding, and/or a negative reaction to anesthesia. Other risks that are more specific to the kyphoplasty procedure include:
- Bone cement leakage. Sometimes the injected bone cement moves beyond the vertebral compression cracks for which it was intended, but this rarely causes any complications even when it occurs. Compared to a similar procedure called vertebroplasty, kyphoplasty has a lower risk for cement leakage but does not appear to have a lower risk for complications. While bone cement is injected with less pressure during kyphoplasty (and thus more likely to stay within the space of the inflated balloon), the cement leakage that occurs more often with vertebroplasty is still typically minor and unlikely to cause symptoms.
- Paralysis. This serious but extremely rare complication can occur in various ways during kyphoplasty if the spinal cord or a nerve root becomes damaged. For example, paralysis could result from a malpositioned instrument during the surgery, or from bone cement that excessively leaks onto the spinal cord or a nerve root.
- Pain persists or worsens. In some cases, kyphoplasty either fails to relieve the pain or results in worse pain or other symptoms. For example, if bone cement leaks onto a nerve root or the spinal cord, it could potentially cause worsened symptoms of pain, tingling, numbness, and/or weakness.
- Pulmonary embolism. If bone cement gets into a vertebral vein, it can potentially travel to the lung and cause an artery obstruction.
- Allergic reaction to bone cement or other agents. It is possible to have an allergic reaction to one of the agents used in kyphoplasty, such as the bone cement (PMMA) or the solution used to see the balloon via x-ray.
It is not yet known whether having kyphoplasty (or vertebroplasty) at one level of the spine increases the risk for a compression fracture at an adjacent spinal level. In general, someone who has a vertebral compression fracture due to osteoporosis is already at an increased risk for having these fractures at other spinal levels, which may explain why someone who has had kyphoplasty (or vertebroplasty) appears to be at an increased risk for future compression fractures at other spinal levels.
See Vertebroplasty vs. Kyphoplasty
Kyphoplasty Risk Factors
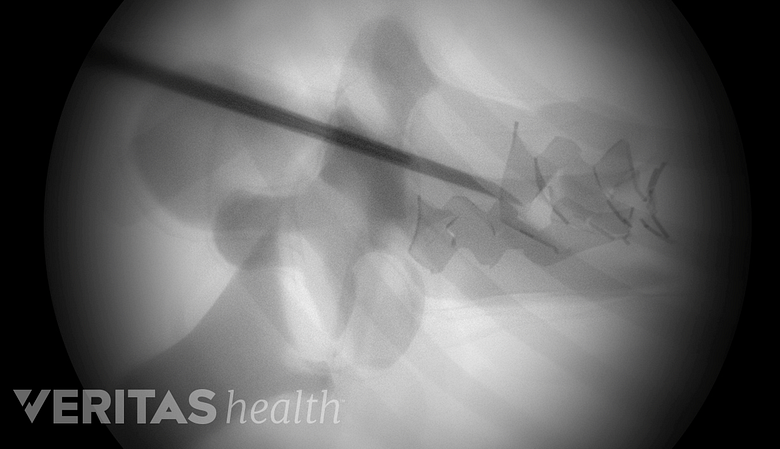
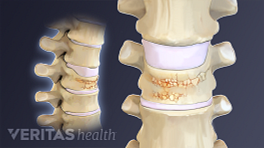
Fluoroscopy is crucial in kyphoplasty for accurate needle placement and cement containment.
Some common factors that might increase the risk of experiencing symptomatic complications from kyphoplasty include:
- Amount of time before having the procedure. Some studies have shown that kyphoplasty has better results when performed less than 8 weeks after the fracture occurs. Typically, kyphoplasty will not be performed 12 or more weeks after the fracture because restoration of vertebral height cannot be achieved after the bone has started to significantly heal.
- Type of fluoroscopy equipment. The fluoroscopy, or x-ray guidance, used in kyphoplasty is crucial to the procedure’s success as the surgeon needs to see where the needle is going and ensure the bone cement is staying within the vertebral fracture. Mobile fluoroscopy equipment, such as the type commonly used in hospital operating rooms, tends to be of lower quality and could result in poorer kyphoplasty outcomes on average.
- Cause of vertebral compression fracture. Vertebral compression fractures resulting from osteoporosis tend to respond better to kyphoplasty (and vertebroplasty) than vertebral fractures caused by cancer. Kyphoplasty complication rates may be twice as high when the vertebral compression fracture is caused by cancer (10%) compared to osteoporosis (4%). 1 Wong C, McGirt MJ. Vertebral compression fractures: a review of current management and multimodal therapy. J Multidiscip Healthc. 2013; 6: 205-14.
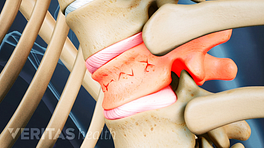
- Shape of the fracture. A vertebral compression fracture at the front of the vertebral body, commonly referred to as a wedge fracture, tends to be most common and responds best to kyphoplasty or vertebroplasty treatments. Other fracture shapes, such as biconcave fractures (middle part of vertebral body is compressed but front and back are intact) or crush fractures (entire vertebral body breaks) are not as likely to have positive outcomes from kyphoplasty.
Several other risk factors for kyphoplasty also exist, such as the surgeon’s skill level and familiarity with the procedure.
- 1 Wong C, McGirt MJ. Vertebral compression fractures: a review of current management and multimodal therapy. J Multidiscip Healthc. 2013; 6: 205-14.