The majority of uncomplicated lower back pain and neck pain typically does not require a precise diagnosis to allow effective treatment to begin. However, if the initial treatment is not helpful or the patient has a more complex underlying medical cause, then obtaining an accurate diagnosis will allow the treatment(s) to be specifically tailored.
In This Article:
- Getting an Accurate Back Pain Diagnosis
- Commonly Confused Terms In Diagnosing Spinal Pain
Diagnostic Process
The medical diagnosis, also called a clinical diagnosis, serves to identify the underlying cause of the neck or back pain. Medical professionals determine the cause of pain through a combination of the following steps:
Review of the patient's medical history
The physician asks a series of questions, such as a description of when the pain and other symptoms started, how it feels, and what activities or treatments make the pain feel better or worse. A thorough review of the medical records and history is also conducted.
Physical examination
Physical evaluation includes testing the range of motion for joint mobility and alignment.
A physical evaluation is performed in the clinic, which is likely to include multiple elements of a comprehensive exam:
- Visual inspection of the overall posture and skin overlying the affected area
- Hands-on inspection by palpating for tender areas and muscle spasm
- Range of motion tests to check mobility and alignment of the involved joints
- Segmental examination to check each spinal segment for proper motion
- Neurological examination, including tests of muscle strength, skin sensation, reflexes, and cranial nerves.
Assessment of the nearby joints and areas that could be masquerading as back pain or contributing to it, such as the hip, sacroiliac joint, and the first rib, among others are typically performed in a physical exam.
Diagnostic testing
In cases when more information is needed, additional studies may be requested, such as diagnostic imaging, electrodiagnostic testing, and/or diagnostic injections.
Based on a detailed history of the patient and an in-person physical examination, most causes of nonspecific neck and/or back pain can be diagnosed and treatment started—without the need for additional diagnostic tests. However, if a patient does not respond to initial treatment, which usually includes physical therapy, medications, ice, heat, ergonomic modification, and activity modification, further testing is indicated.
Diagnostic Imaging
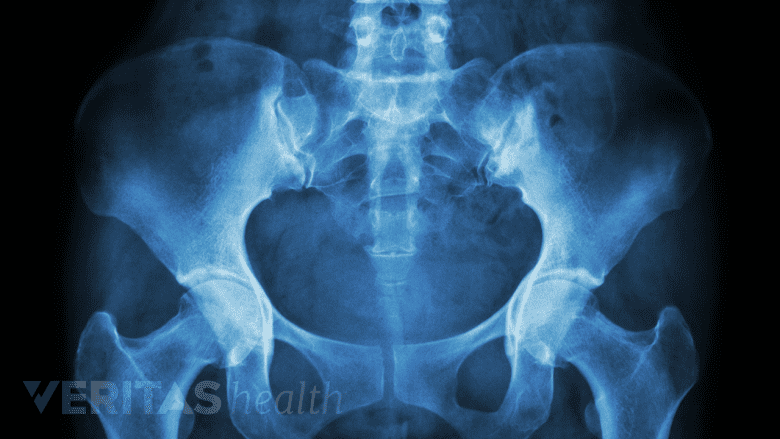
X-rays assist in diagnosing pain by detecting degenerative changes, and fractures.
The most common diagnostic imaging studies for neck and back pain include:
- X-ray, which shows details of the bony structures in the spine. An x-ray particularly useful in identifying degenerative changes or fractures and can help identify certain types of rheumatological causes of pain (such as osteoarthritis). Flexion and extension X-rays may also be ordered if spinal instability is suspected.
- MRI scan, which is a common option for assessing the spine and its soft tissues, such as the discs and nerve roots. MRI scans may also help distinguish a chronic condition from an acute problem in certain situations. In analyzing a spine with a history of previous surgery, MRI’s are usually performed after a contrast dye is injected to better view blood flow in the region being studied.
- CT scan, which uses radiation to create a series of cross-section images by a computer. To get a better view of the soft tissues, especially if an MRI is not an option, sometimes a CT scan is performed with a contrast dye injected into the spinal canal (CT/myelogram).
Less commonly, other types of diagnostic imaging may be considered for a more detailed analysis of tissues. These imaging techniques may include:
- Bone scan, a nuclear imaging study commonly used to help find and track the extent of bone-related issues, such as fractures, tumors, infections, and unexplained bone pain.
- SPECT scan, which uses a computer to assemble cross-sections of nuclear images. SPECT is commonly used with a bone scan when viewing the intricate bones of the spine in order to see more areas and in better detail. SPECT may also be used with CT scans to better view a metabolic abnormality, such as a tumor, and its relation to the bony structures.
- DEXA scan, also called bone densitometry, uses dual-energy x-ray absorptiometry to measure the density of bones. This scan is commonly used to assess the risk of osteoporosis and small fractures in the vertebrae.
In some cases, several imaging scans are used as part of the diagnostic process for neck or back pain.
Electrodiagnostic Testing
An electrodiagnostic study for neck or back pain typically involves the following two tests:
- Nerve conduction studies (NCS) measure how fast the nerve is conducting electrical signals. If an unusual slowdown is detected, then that part of the nerve is likely experiencing dysfunction.
- Electromyography (EMG) measures the electrical activity within a muscle. Typically, a needle electrode is inserted into different muscles to determine which ones may be weak and to what extent, as well as the muscle fiber’s interaction with the nerve that connects to it.
An EMG is often performed after NCS. These tests provide complementary information, which is much more useful than either test alone.
If spinal cord dysfunction is suspected, somatosensory evoked potentials (SSEP) may also be requested.
Diagnostic Injections
Facet joint injections reduce inflammation and control painful symptoms.
Diagnostic injections may be useful in pinpointing a specific anatomical structure as the pain source. General guidelines for using diagnostic injections are:
- All of these injections must use fluoroscopy (live x-ray guidance) and contrast dye to visualize exactly where the needle is placed within the spine, providing additional procedural safety and making sure the targeted structure is accurately injected.
- Most commonly, a combination of a numbing agent (anesthetic) and corticosteroid is injected.
- If complete pain relief is experienced for the duration of the local anesthetic action, then it is most likely that the presumptive source of pain has been identified.
- Repeat injection using a different duration of anesthetic medication may be necessary if the patient does not get long term relief and an invasive procedure may be contemplated.
If the patient experiences only partial relief for the duration of the local anesthetic action, then the patient likely has an additional source of pain contributing to their overall pain picture and additional injections or other treatments may be considered.
Common diagnostic injections include:
- Facet joint injection. This procedure involves injecting lidocaine (anesthetic medication) and a steroid into a facet joint suspected of causing pain. It may be performed as a diagnostic test as well as to help provide pain relief.
- Medial branch block. This procedure involves injecting lidocaine solution onto the sensory nerve that innervates the facet joint. This injection is purely diagnostic to check if the facet joint may be responsible for pain.
- Selective nerve root block. This procedure involves injecting an anesthetic and corticosteroid solution around a specific nerve root that is a suspected source of pain.
Other injections that may be considered for diagnostic purposes include lumbar sympathetic nerve blocks, sacroiliac joint blocks, and stellate ganglion blocks, among others. In cases of suspicion of an adjacent joint contributing to the overall pain picture, that joint can be blocked as well utilizing appropriate techniques, which may include fluoroscopy or ultrasound guidance depending on the specific structure targeted.
Read more: Introduction to Diagnostic Studies for Back and Neck Pain
Editor’s Top Picks

