Many terms may be used to describe issues with a spinal disc and disc pain, and all may be used differently and, at times, interchangeably. Some commonly used terms include:
- Herniated disc
- Pinched nerve
- Ruptured/ torn disc
- Bulging disc
- Disc protrusion
- Slipped disc
There is no main consensus on the use of these terms, and it can be frustrating to hear one diagnosis described in many different ways.
The medical diagnosis identifies the underlying cause of back pain, leg pain, and other symptoms. It is more useful to gain a clear understanding of the medical diagnosis than to sort through various medical terms.
In This Article:
- What's a Herniated Disc, Pinched Nerve, Bulging Disc...?
- Herniated Disc vs. Degenerative Disc Disease Treatments
- Herniated Disc Video
Two Causes of Pain: Pinched Nerve vs. Disc Pain
There are two main ways a spinal disc can cause pain:
Pinched nerve

A herniated disc may compress the nearby nerve root, causing radicular pain.
In many cases a herniated disc itself is not painful, but rather the material leaking out of the disc pinches, inflames, or irritates a nearby nerve, causing radicular pain. Radicular pain (also called nerve root pain), describes sharp, shooting pains that radiate to other parts of the body, such as from the low back down the leg or from the neck down the arm. Leg pain from a pinched nerve is commonly called sciatica.
Disc pain
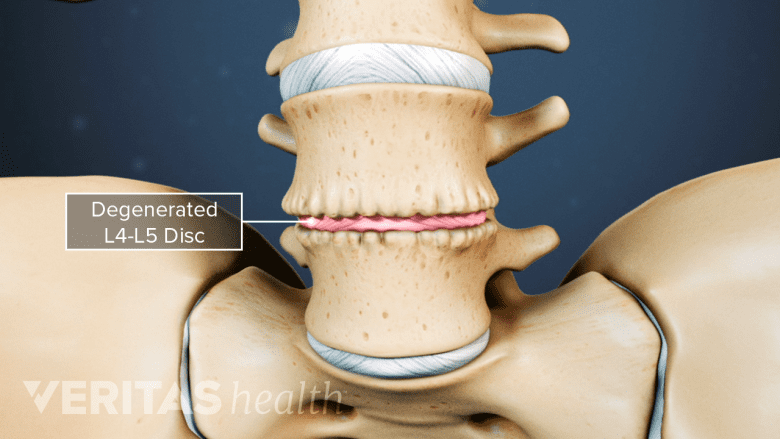
Age-related disc degeneration can cause pain and instability in the spine.
A spinal disc itself may be the source of pain if it dehydrates or degenerates to the point of causing pain and instability in the spinal segment (called degenerative disc disease). Degenerative disc pain tends to include a chronic, low-level pain around the disc and occasional episodes of more severe pain.
A herniated disc and degenerative disc disease typically occur in the cervical spine (neck) and lumbar spine (lower back). Disc pain tends to be most common in the lower back, where most of the movement and weight-bearing in the spine occurs. These conditions are uncommon in the mid-back (the thoracic spine).