Klippel-Feil syndrome (KFS) is a congenital bone condition in which at least 2 vertebrae in the cervical spine remain fused and immobile. Depending on how many vertebrae remain fused and/or the location of the congenital fusions, neck pain symptoms can vary from mild to severe with the possibility of many other associated abnormalities in other areas of the body.
In This Article:
- What to Know About Klippel-Feil Syndrome
- Klippel-Feil Symptoms and Associated Conditions
- Klippel-Feil Syndrome Diagnosis
- Klippel-Feil Syndrome Treatment
3 Classic Signs of KFS
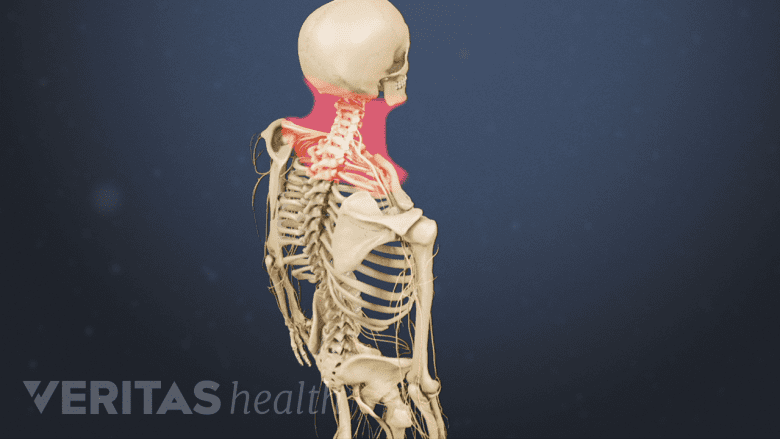
Limited neck mobility is a cardinal sign of Klippel-Feil syndrome.
In most cases, people with KFS have at least 1 of the following 3 signs:
- Visibly short neck
- Low hairline behind the head
- Reduced neck mobility
Fewer than 50% of people with KFS have all 3 of these classic signs.1Klippel-Feil syndrome. U.S. National Library of Medicine, Genetics Home Reference Web site. https://ghr.nlm.nih.gov/condition/klippel-feil-syndrome. Updated June 2015. Accessed February 26, 2018.
The Course of KFS
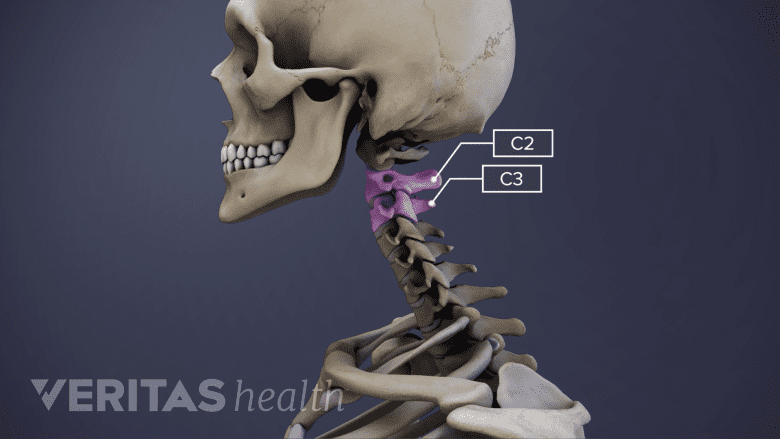
Klippel-Feil syndrome often causes fusion at C2-C3 in the cervical spine.
Klippel-Feil syndrome is present from birth and lasts for the duration of life. According to some estimates, about 1 in 40,000 people have KFS.1Klippel-Feil syndrome. U.S. National Library of Medicine, Genetics Home Reference Web site. https://ghr.nlm.nih.gov/condition/klippel-feil-syndrome. Updated June 2015. Accessed February 26, 2018.
KFS is not always noticed at birth or even during childhood. If the case is mild or accompanied by other conditions that need more immediate medical attention, KFS may go years or decades before it is diagnosed.
In general, the cervical spine is more mobile closer to the skull. If only 2 vertebrae are congenitally fused lower in the less-mobile area of the cervical spine, such as at where C6 and C7 would normally be, there might not be any obvious signs of Klippel-Feil syndrome.
If instead KFS presents with 1 or more congenital fusions near the skull, signs, and symptoms tend to be more severe with even less neck mobility, which may cause more stress on nearby joints, muscles, and other soft tissues. The C2-C3 level, which is near the top of the cervical spine, is the most common congenital fusion found with KFS.2Klippel-Feil syndrome. National Center for Advancing Translational Sciences, Genetic and Rare Diseases Information Center. https://rarediseases.info.nih.gov/diseases/10280/klippel-feil-syndrome. Accessed February 26, 2018.
See All About the C2-C5 Spinal Motion Segments
KFS tends to cause more symptoms as the body continues to grow and age. For example, osteoarthritis typically develops around the congenital fusions, leading to bone spurs growing and potentially compressing a nearby nerve root and/or the spinal cord.
There is currently no cure for KFS, so treatments focus on managing the symptoms and offering support.
KFS Causes
Klippel-Feil syndrome starts sometime between the 3rd and 8th week of development within the womb, which is the time period when the spine normally starts to develop and divide into segments. During this stage, KFS can occur when some vertebrae in the cervical spine fail to divide into separate segments.
The exact mechanisms of what causes KFS are still being studied. In general, there are two ways KFS occurs:
- Sporadic. Most commonly, KFS occurs without any family history or known genetic component.
- Genetic mutation. Sometimes one or more genetic mutations may be involved in the development of KFS. For example, mutations in GDF3, GDF6, and/or MEOX1 genes have all been linked to KFS. These genes are all involved in bone development, but it is not known how these mutations specifically cause cervical vertebrae not to divide.
Sometimes KFS develops as a secondary feature of another condition, such as Wildervanck syndrome or fetal alcohol syndrome.
KFS Classifications
Klippel-Feil syndrome was first reported by Maurice Klippel and Andrew Feil in 1912. The original classification system for KFS described by Feil involved:
- Type I. Extensive fusion of most or all of the cervical spine.
- Type II. Fusion or only 1 or 2 vertebrae in the cervical spine.
- Type III. Fusion exists in part of the thoracic and/or lumbar spine, in addition to Type I or Type II KFS.
Other classifications have also been developed in the years since, such as classifications that take into account different gene mutations.3Clarke RA, Catalan G, Diwan AD, Kearsley JH. Heterogeneity in Klippel-Feil syndrome: a new classification. Pediatr Radiol. 1998; 28(12):967-74.
When Klippel-Feil Syndrome Is Serious

Klippel-Feil syndrome, along with cervical myelopathy, may require immediate medical attention.
Some cases of KFS can become serious and potentially life-threatening in a few different ways:
- Cervical myelopathy. If the spinal cord starts to become compressed, such as from bony overgrowths or severe spinal deformity, problems with coordination and reduced control over bodily functions could result.
- Spinal fragility. A severe cervical spine instability and/or weakness, such as brittle bone or a hole that exposes the spinal cord, makes the neck more susceptible to serious injury. For example, a relatively minor accident that causes most people temporary pain, such as a sports collision, could instead result in a broken neck (and possibly paralysis or even death).4Vaidyanathan S, Hughes PL, Soni BM, Singh G, Sett P. Klippel-Feil syndrome - the risk of cervical spinal cord injury: a case report. BMC Fam Pract. 2002; 3:6.
In addition, sometimes KFS is accompanied by other serious abnormalities, such as heart and/or lung problems. Some of these associated disorders have the potential to become life-threatening by themselves and must be monitored with regular doctor visits.
- 1 Klippel-Feil syndrome. U.S. National Library of Medicine, Genetics Home Reference Web site. https://ghr.nlm.nih.gov/condition/klippel-feil-syndrome. Updated June 2015. Accessed February 26, 2018.
- 2 Klippel-Feil syndrome. National Center for Advancing Translational Sciences, Genetic and Rare Diseases Information Center. https://rarediseases.info.nih.gov/diseases/10280/klippel-feil-syndrome. Accessed February 26, 2018.
- 3 Clarke RA, Catalan G, Diwan AD, Kearsley JH. Heterogeneity in Klippel-Feil syndrome: a new classification. Pediatr Radiol. 1998; 28(12):967-74.
- 4 Vaidyanathan S, Hughes PL, Soni BM, Singh G, Sett P. Klippel-Feil syndrome - the risk of cervical spinal cord injury: a case report. BMC Fam Pract. 2002; 3:6.

