Isthmic spondylolisthesis is typically diagnosed in people of working age. Several causes and risk factors have been postulated for this condition, but there is no clear consensus on the exact causes or risk factors.1Kinzyagulov BR, Lebedev VB, Zuev AA. Isthmic spondylolisthesis: the current state of the problem. Nejrohirurgiâ (Mosk). 2022;24(4):101-110. doi:10.17650/1683-3295-2022-24-4-101-10
In This Article:
- Isthmic Spondylolisthesis
- Isthmic Spondylolisthesis Symptoms
- Understanding the Causes and Diagnosis of Isthmic Spondylolisthesis
- Nonsurgical Treatment for Isthmic Spondylolisthesis
- Spinal Fusion Surgery for Isthmic Spondylolisthesis
- Isthmic Spondylolisthesis Video
Potential Causes and Risk Factors for Isthmic Spondylolisthesis
Limited evidence suggests that isthmic spondylolisthesis may have a genetic origin.
Some of the causes and risk factors of isthmic spondylolisthesis based on the available literature are described below:
- Repetitive stress from occupational or recreational activities. Isthmic spondylolisthesis is often associated with sports that require repetitive hyperextension of the lumbar spine. Individuals who often engage in activities such as weightlifting, gymnastics, and wrestling are at a higher risk of developing the condition.2Mohile NV, Kuczmarski AS, Lee D, Warburton C, Rakoczy K, Butler AJ. Spondylolysis and isthmic spondylolisthesis: a guide to diagnosis and management. J Am Board Fam Med. 2022;35(6):1204-1216. doi:10.3122/jabfm.2022.220130R1
- Genetics. There is some evidence to suggest that isthmic spondylolisthesis may be hereditary, with a higher incidence of the condition seen in certain families.3McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
- Trauma. Isthmic spondylolisthesis can also be caused high energy trauma, such as a car crash or work-related accidents in factories where the lower back is hit by a heavy object. In this case, the condition may also be called traumatic lumbar spondylolisthesis.4Konan LM, Davis DD, Mesfin FB. Traumatic Lumbar Spondylolisthesis. [Updated 2022 Aug 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448159/
- Congenital defects. Some people may be born with a defect in the pars interarticularis, which can increase the risk of developing isthmic spondylolisthesis later in life. In such cases, the condition may also be called congenital spondylolisthesis.5Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
- Age. Isthmic spondylolisthesis is more likely to develop in kids around 6 years of age or in early adulthood.6Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560679/,7Mikhael MM, Shapiro GS, Wang JC. High-grade adult isthmic L5-s1 spondylolisthesis: a report of intraoperative slip progression treated with surgical reduction and posterior instrumented fusion. Global Spine J. 2012;2(2):119-124. doi:10.1055/s-0032-1307257
- Gender. Men are three times more likely to develop isthmic spondylolisthesis than women.5Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
While these factors may increase the risk of developing isthmic spondylolisthesis, it is important to note that not everyone who has these risk factors will develop the condition. It is also possible to develop isthmic spondylolisthesis without any known risk factors.
How Isthmic Spondylolisthesis Is Diagnosed: Clinical and Radiographic Tests
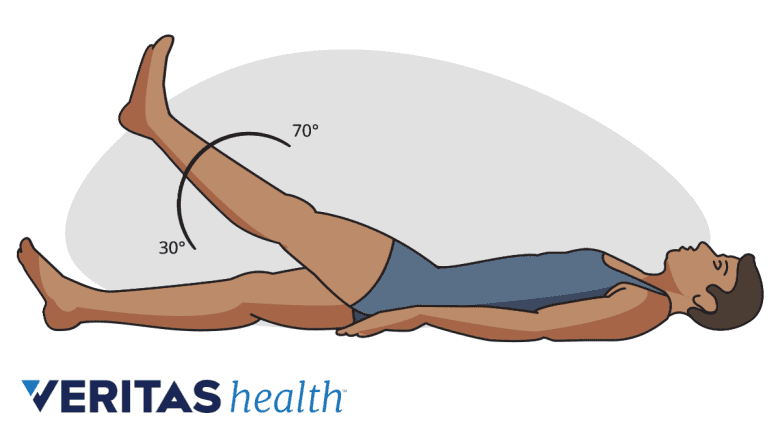
A positive straight leg raise test may indicate nerve root impingement in isthmic spondylolisthesis.
While diagnosing isthmic spondylolisthesis, physicians check for a few classic symptoms and signs of the condition, such as6Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560679/,8Kreiner DS, Baisden J, Mazanec DJ, et al. Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of adult isthmic spondylolisthesis. The Spine Journal. 2016;16(12):1478-1485. doi:10.1016/j.spinee.2016.08.034:
- A history of lower back pain with or without sciatica (back pain and leg pain)
- A positive straight leg raise test, which includes the patient lying on his/her back and lifting one leg at a time with the other leg flat or bent at the knee. A pain encountered while lifting the affected leg usually indicates spinal nerve compression/sciatica
- Pain with hyperextension, or bending backwards
- Stiffness while bending the spine forward or backward
- Tightness in the hamstring muscles
If isthmic spondylolisthesis is suspected, radiographic tests may be ordered. Radiographic tests for isthmic spondylolisthesis
Radiographic tests for isthmic spondylolisthesis

X-rays and CT scans are considered reliable tests in confirming isthmic spondylolisthesis.
X-rays and/or computed tomography (CT) scans are usually considered reliable diagnostic tests to confirm isthmic spondylolisthesis and locate the accurate level of the affected vertebrae in the spine.
If nerve impingement is suspected, a magnetic resonance imaging (MRI) scan may be recommended.8Kreiner DS, Baisden J, Mazanec DJ, et al. Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of adult isthmic spondylolisthesis. The Spine Journal. 2016;16(12):1478-1485. doi:10.1016/j.spinee.2016.08.034
Bone scan with or without single-photon emission computerized tomography (SPECT) imaging can also be helpful determining the chronicity of the condition.9Matesan M, Behnia F, Bermo M, Vesselle H. SPECT/CT bone scintigraphy to evaluate low back pain in young athletes: common and uncommon etiologies. J Orthop Surg Res. 2016 Jul 7;11(1):76. doi: 10.1186/s13018-016-0402-1. PMID: 27387155; PMCID: PMC4936246.
- 1 Kinzyagulov BR, Lebedev VB, Zuev AA. Isthmic spondylolisthesis: the current state of the problem. Nejrohirurgiâ (Mosk). 2022;24(4):101-110. doi:10.17650/1683-3295-2022-24-4-101-10
- 2 Mohile NV, Kuczmarski AS, Lee D, Warburton C, Rakoczy K, Butler AJ. Spondylolysis and isthmic spondylolisthesis: a guide to diagnosis and management. J Am Board Fam Med. 2022;35(6):1204-1216. doi:10.3122/jabfm.2022.220130R1
- 3 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
- 4 Konan LM, Davis DD, Mesfin FB. Traumatic Lumbar Spondylolisthesis. [Updated 2022 Aug 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448159/
- 5 Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
- 6 Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560679/
- 7 Mikhael MM, Shapiro GS, Wang JC. High-grade adult isthmic L5-s1 spondylolisthesis: a report of intraoperative slip progression treated with surgical reduction and posterior instrumented fusion. Global Spine J. 2012;2(2):119-124. doi:10.1055/s-0032-1307257
- 8 Kreiner DS, Baisden J, Mazanec DJ, et al. Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of adult isthmic spondylolisthesis. The Spine Journal. 2016;16(12):1478-1485. doi:10.1016/j.spinee.2016.08.034
- 9 Matesan M, Behnia F, Bermo M, Vesselle H. SPECT/CT bone scintigraphy to evaluate low back pain in young athletes: common and uncommon etiologies. J Orthop Surg Res. 2016 Jul 7;11(1):76. doi: 10.1186/s13018-016-0402-1. PMID: 27387155; PMCID: PMC4936246.

