Muscle relaxers help reduce pain, improve function, and promote healing when used in the treatment of back and neck pain.1Barreto TW, Lin KW. Noninvasive Treatments for Low Back Pain. American Family Physician. 2017;96(5):324-327. Accessed August 14, 2023. https://www.aafp.org/pubs/afp/issues/2017/0901/p324.html
In This Article:
- Muscle Relaxants: List of Common Muscle Relaxers
- Side Effects and Risks of Muscle Relaxers
- Common Uses for Treating Back and Neck Pain with Muscle Relaxers
- Medications for Back Pain Video
Muscle Relaxers for Back Pain from Trauma
Muscle relaxers are used to alleviate muscle spasms caused by spinal trauma.
Damage to muscle tissue from an injury or strain, such as lifting a heavy object or twisting in an awkward position, can cause muscle spasms as a natural form of protection. The body responds to the injury by sending signals to contract the muscles in order to prevent movement or additional stress.2Gash MC, Kandle PF, Murray IV, et al. Physiology, Muscle Contraction. [Updated 2023 Apr 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537140/
Muscle relaxers with antispasmodic activity, such as carisoprodol and tizanidine, are typically prescribed in such cases.3Chou R, Peterson K, Helfand M. Comparative efficacy and safety of skeletal muscle relaxants for spasticity and musculoskeletal conditions: a systematic review. J Pain Symptom Manage. 2004;28(2):140-175. doi:10.1016/j.jpainsymman.2004.05.002
Taking rest and using non-drug therapies, such as massage therapy or heat therapy, are generally recommended in addition to taking muscle relaxers for enhanced healing and long-term improvement.1Barreto TW, Lin KW. Noninvasive Treatments for Low Back Pain. American Family Physician. 2017;96(5):324-327. Accessed August 14, 2023. https://www.aafp.org/pubs/afp/issues/2017/0901/p324.html
Muscle Relaxers for Nerve Pain in the Back and Leg
Antispasmodic muscle relaxers provide relief from severe sciatica pain.
Nerve compression (pinched nerves) in the spine can cause burning pain (sciatica) and muscle spasms in the back and/or legs by impacting the ability of the nerves to send proper signals to certain muscles.4Davis D, Maini K, Vasudevan A. Sciatica. [Updated 2022 May 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507908/
Muscle relaxers with antispasmodic effects provide relief from severe pain or disability in such cases. However, these medications do not address the underlying cause of nerve compression, such as a herniated disc or spinal stenosis, and only mask the symptoms.1Barreto TW, Lin KW. Noninvasive Treatments for Low Back Pain. American Family Physician. 2017;96(5):324-327. Accessed August 14, 2023. https://www.aafp.org/pubs/afp/issues/2017/0901/p324.html
Muscle Relaxers for Spinal Cord Injuries and Neurologic Disorders
Muscle contraction (tightening) and relaxation are regulated by the spinal cord, and injury or damage to the spinal cord causes muscle spasticity (prolonged muscle tightening).5Rivelis Y, Zafar N, Morice K. Spasticity. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507869/
Similarly, the spinal cord is a major component of the nervous system, and certain neurological disorders (eg, multiple sclerosis, cerebral palsy, and stroke) cause spasticity to develop.5Rivelis Y, Zafar N, Morice K. Spasticity. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507869/
Muscle relaxers with antispastic effects, such as baclofen and dantrolene, reduce spasticity and improve functioning for people with these conditions.6Dietz N, Wagers S, Harkema SJ, D'Amico JM. Intrathecal and Oral Baclofen Use in Adults With Spinal Cord Injury: A Systematic Review of Efficacy in Spasticity Reduction, Functional Changes, Dosing, and Adverse Events. Arch Phys Med Rehabil. 2023;104(1):119-131. doi:10.1016/j.apmr.2022.05.011
Using Muscle Relaxers to Improve Sleep in Back and Neck Pain
Certain muscle relaxers are used to address sleep difficulties caused by back or neck pain. Taking a muscle relaxer with sedating effects around bedtime alleviates pain and/or discomfort and promotes sleepiness.7Lederman S, Arnold LM, Vaughn B, Kelley M, Sullivan GM. Efficacy and Safety of Sublingual Cyclobenzaprine for the Treatment of Fibromyalgia: Results From a Randomized, Double-Blind, Placebo-Controlled Trial [published online ahead of print, 2023 May 11]. Arthritis Care Res (Hoboken). 2023. doi:10.1002/acr.25142
Additional Medications and Therapies for Back and Neck Pain
While muscle relaxers serve as an effective method for addressing back and neck pain, numerous alternative strategies exist to manage pain and disability without the need for a prescription. These non-prescription approaches encompass a wide range of options, including medication, exercise, and lifestyle modifications.
Over-the-counter (OTC) medications for back and neck pain
NSAIDs provide anti-inflammatory effects and help calm inflammation and pain in the neck.
OTC products can be taken orally for overall pain relief or applied locally to treat pain in a specific area. These medications include:
- Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil) and naproxen (Aleve), which help reduce inflammation and relieve pain
- Acetaminophen (Tylenol), which helps reduce pain but does not reduce inflammation
- Topical counterirritants, such as Icy Hot, Bengay, Biofreeze, Tiger Balm or Aspercreme, which contain pain-relieving ingredients, such as camphor, menthol, and capsaicin, to help reduce pain when applied locally
- Natural anti-inflammatory creams, such as Blue Emu (glucosamine and dimethyl sulfone) and Arnica Pain Relief (arnica montana plant), help reduce inflammation and ease pain
- Lidocaine patches, such as Salonpas and Aspercreme with lidocaine, provide pain relief by numbing the area to which it is applied
- Cannabidiol (CBD) products, such as Hempvana or CBD gummies, are applied locally or taken orally to provide mild pain relief
It is important to note that some medications are not suitable for all patients due to the potential risk of gastric irritation, cardiac problems, or other side effects. To avoid these risks, consulting a physician before taking these medications is advisable.
Alternative therapies for back and neck pain
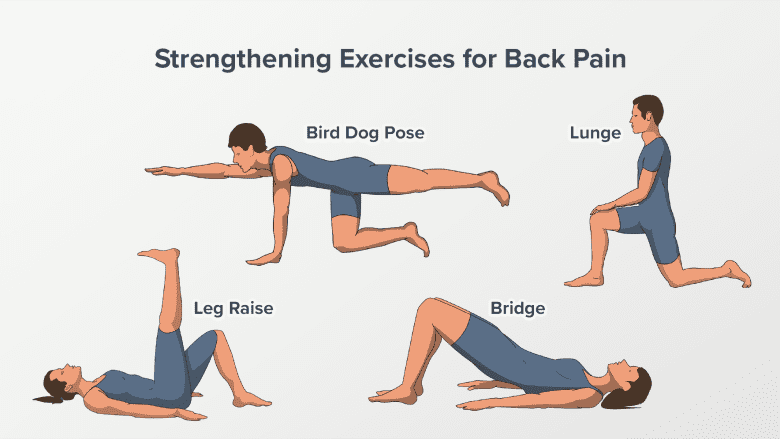
Strengthening exercises ease back pain by improving muscle strength and spinal stability.
Alternative strategies for managing back and neck pain address the underlying causes and the psychological components of pain, including8Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Annals of Internal Medicine. 2017;166(7):514. doi:10.7326/m16-2367:
- Physical therapy
- Exercise and strength training
- Yoga
- Massage therapy
- Heat and cold therapy
- Postural modifications
- Weight management (if appropriate)
- Sleep hygiene
The effectiveness of these therapies varies from person to person. It is advisable to consult with a doctor or qualified healthcare professional to determine which strategies are safe.
- 1 Barreto TW, Lin KW. Noninvasive Treatments for Low Back Pain. American Family Physician. 2017;96(5):324-327. Accessed August 14, 2023. https://www.aafp.org/pubs/afp/issues/2017/0901/p324.html
- 2 Gash MC, Kandle PF, Murray IV, et al. Physiology, Muscle Contraction. [Updated 2023 Apr 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537140/
- 3 Chou R, Peterson K, Helfand M. Comparative efficacy and safety of skeletal muscle relaxants for spasticity and musculoskeletal conditions: a systematic review. J Pain Symptom Manage. 2004;28(2):140-175. doi:10.1016/j.jpainsymman.2004.05.002
- 4 Davis D, Maini K, Vasudevan A. Sciatica. [Updated 2022 May 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507908/
- 5 Rivelis Y, Zafar N, Morice K. Spasticity. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507869/
- 6 Dietz N, Wagers S, Harkema SJ, D'Amico JM. Intrathecal and Oral Baclofen Use in Adults With Spinal Cord Injury: A Systematic Review of Efficacy in Spasticity Reduction, Functional Changes, Dosing, and Adverse Events. Arch Phys Med Rehabil. 2023;104(1):119-131. doi:10.1016/j.apmr.2022.05.011
- 7 Lederman S, Arnold LM, Vaughn B, Kelley M, Sullivan GM. Efficacy and Safety of Sublingual Cyclobenzaprine for the Treatment of Fibromyalgia: Results From a Randomized, Double-Blind, Placebo-Controlled Trial [published online ahead of print, 2023 May 11]. Arthritis Care Res (Hoboken). 2023. doi:10.1002/acr.25142
- 8 Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Annals of Internal Medicine. 2017;166(7):514. doi:10.7326/m16-2367

