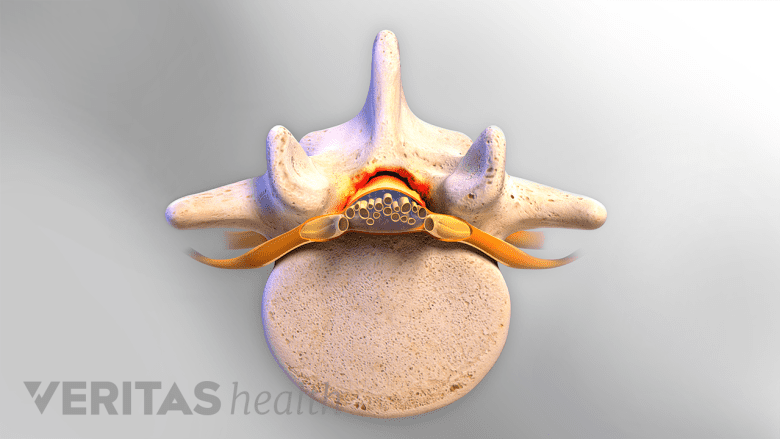
Spinal stenosis occurs when one or more bony openings (foramina) within the spine begin to narrow and reduce space for the nerves. This process can occur within the spinal canal (where the spinal cord runs down the center) and/or in the intervertebral foramina where spinal nerves exit the spinal canal. Depending on the location and how much narrowing occurs over time, a spinal nerve or the spinal cord could become compressed and cause pain, tingling, numbness, and/or weakness.
In This Article:
Range of Spinal Stenosis Signs and Symptoms

Spinal stenosis can cause pain, numbness, and weakness in the back, neck, and limbs.
Spinal stenosis can greatly vary from person to person. Signs and symptoms may include one or more of the following:
- Pain. The pain might be dull and confined to the neck or lower back, or it could be an electric-like pain that radiates into the arm(s) or leg(s). The pain can vary over time, possibly flaring up during certain activities. Sometimes the pain is more of a pins-and-needles tingling sensation.
- Numbness. Reduced sensation or total numbness may occur in the arm, leg, and/or other areas of the body.
- Weakness. Reduced strength or problems with coordination may be experienced in the arm, leg, and/or other parts of the body. Severe compression of the spinal cord or cauda equina (nerve roots running below the spinal cord) could result in bowel and/or bladder dysfunction.
Spinal stenosis does not always cause pain. While rare, numbness or weakness might be present with little or no pain.
Common Causes
Spinal stenosis is typically caused by one or more of the following factors:
Spinal osteoarthritis
When the smooth cartilage covering the facet joints (which connect the backs of adjacent vertebrae) start to break down, bones begin to rub against each other and may lead to the formation of abnormal bone growth, called osteophytes or bone spurs. The resulting inflammation and osteophyte formation can contribute to narrowing of the foramina. (A similar process is responsible for osteoarthritis leading to enlargement of knuckles in the hand.)
Degenerative disc disease
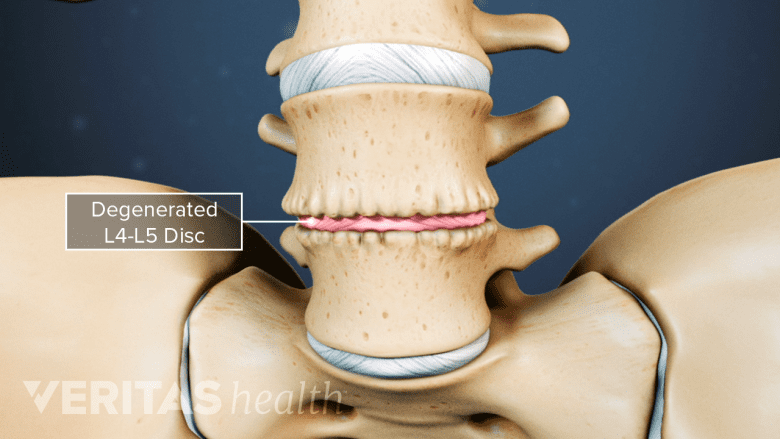
Degenerated discs can press into the spinal canal and exacerbate loss of facet joint cartilage.
When discs lose hydration and start to flatten, the intervertebral foramina also start to narrow. A disc bulge can also start to push into the spinal canal. Disc degeneration can also put more pressure on the facet joints and accelerate their degeneration as well.
See What Is Degenerative Disc Disease?
Ligament thickening or buckling
Ligaments in the spinal canal can ossify (thicken and turn into bony tissue) and encroach upon the spinal cord or nearby spinal nerves. Some ligaments may also become more susceptible to buckling into the spinal canal as spinal degeneration progresses.
Other factors may also contribute to spinal stenosis, such as spinal deformity or cyst growths.
The Course of Spinal Stenosis
The progression of spinal stenosis varies and affects the surgical and nonsurgical treatment options considered.
The narrowing of the foramina in the spine usually develops over time as part of the aging process. While spinal stenosis typically occurs in people age 50 or older, it can also develop sooner due to injury or from birth (congenital factors).1Spinal Stenosis: Who Gets It? National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health Website. https://www.niams.nih.gov/health-topics/spinal-stenosis. Accessed September 23, 2019.,2Spinal Stenosis. Arthritis Foundation Website. https://www.arthritis.org/about-arthritis/types/spinal-stenosis/. Accessed September 23, 2019.
Spinal stenosis may worsen over time, but the rate of progression is variable and may not always produce signs or symptoms.3Majid K. Pathophysiology, clinical presentation, natural history, and review of the SPORT trials. Seminars in Spine Surgery. 2013; 25(4):228-33. doi: 10.1053/j.semss.2013.05.002. While some people may experience progressive worsening of symptoms, others may find that their symptoms are alleviated by physical therapy, medication, short period of rest, or other nonsurgical treatments.4Melancia JL, Francisco AF, Antunes JL. Spinal stenosis. Neurologic Aspects of Systemic Disease Part I. 2014; 541-9. doi:10.1016/b978-0-7020-4086-3.00035-7.
When neurological deficits, such as numbness or weakness, continue to worsen despite rest and nonsurgical treatments, surgery may need to be considered. Surgery is typically recommended for spinal stenosis when imaging and other diagnostic measures show that signs and symptoms are likely to be relieved by decompressing a spinal nerve and/or the spinal cord. Before opting for spinal stenosis surgery, it is important to discuss the potential risks and other treatment options with the surgeon.
When Spinal Stenosis Is Serious
Neurological deficits — such as from radiculopathy, myelopathy, and/or cauda equina syndrome — can develop when spinal stenosis becomes severe. If a spinal nerve or the spinal cord is compressed for long enough, permanent numbness and/or paralysis can occur. It is important to seek immediate medical attention for any numbness or weakness that radiates into the arm(s) or leg(s), or for any problems with coordination or bowel/bladder control.
- 1 Spinal Stenosis: Who Gets It? National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health Website. https://www.niams.nih.gov/health-topics/spinal-stenosis. Accessed September 23, 2019.
- 2 Spinal Stenosis. Arthritis Foundation Website. https://www.arthritis.org/about-arthritis/types/spinal-stenosis/. Accessed September 23, 2019.
- 3 Majid K. Pathophysiology, clinical presentation, natural history, and review of the SPORT trials. Seminars in Spine Surgery. 2013; 25(4):228-33. doi: 10.1053/j.semss.2013.05.002.
- 4 Melancia JL, Francisco AF, Antunes JL. Spinal stenosis. Neurologic Aspects of Systemic Disease Part I. 2014; 541-9. doi:10.1016/b978-0-7020-4086-3.00035-7.

