Having difficulty swallowing, also called dysphagia, is among the most common and concerning aspects of an ACDF recovery. Not only is swallowing critical to how the body naturally gets needed nutrients, it also plays an important role in making mealtime a pleasurable experience. Dysphagia can also be dangerous as it increases the risk for choking.
Most ACDF patients fully recover their ability to swallow within a few days after surgery. Sometimes, however, dysphagia lingers for weeks, months, or even longer. Studies that have followed ACDF patients post-surgery for at least 2 years have found differing results regarding dysphagia. For example, one study estimated that about 10% of ACDF patients have at least some long-lasting issues with swallowing, whereas another study put the number above 30%.1Yang Y, Ma L, Liu H et al. Comparison of the incidence of patient-reported postoperative dysphagia between ACDF with a traditional anterior plate and artificial cervical disc replacement. Clinical Neurology and Neurosurgery. 2016; 148: 72-78.,2Yue WM, Brodner W, Highland TR. Persistent swallowing and voice problems after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year follow-up study. Eur Spine J. 2005;14(7):677-82.
In This Article:
- What to Expect After ACDF Surgery
- After ACDF: Trouble with Swallowing
- After ACDF: Trouble with Speaking
- After ACDF: Managing Mental Health
- After ACDF: How to Prevent or Manage Constipation
How to Manage Dysphagia During Recovery
After ACDF surgery, most patients have a sore throat. To monitor for a potential swallowing problem while in the hospital, patients are started on clear liquids and then progress to soft foods, such as applesauce. ACDF patients typically get to go home one or two days after surgery, so long as no serious complications are detected, such as a severe swallowing problem that could lead to choking.
See Hospital Care After ACDF Surgery
Here are some tips to help manage dysphagia that lingers after returning home from the hospital:
- Stock up on soft foods. Yogurt, applesauce, creamy soups (no chunks), and other soft foods are good choices during the recovery period when swallowing is still difficult.
- Puree hard foods. Using a food processor or blender to breakdown solid foods—such as meat, poultry, veggies, and others—is a good way to keep the calorie count up and maintain protein levels. Remember to add enough liquid so the pureed food slides down easily.
- Use a bendy straw if it helps. Unlike a straight straw, a bendable straw’s angle can be altered to conveniently meet the user’s mouth to minimize head and neck movements.
Risk Factors for Dysphagia
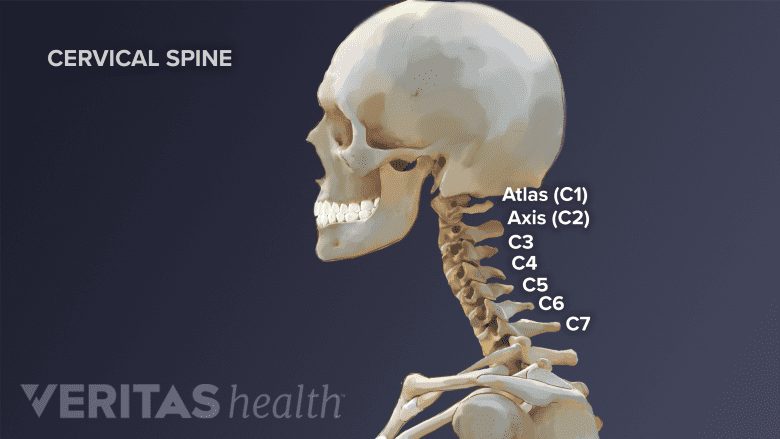
Cervical spine fusion (above C4) may increase the risk of dysphagia after ACDF surgery.
The medical literature has not yet reached a consensus regarding which ACDF patients are at higher risk for developing dysphagia that becomes permanent. However, some studies have found evidence that suggests the following could be risk factors:
- Length of surgery time3Anderson KK, Arnold PM. Oropharyngeal Dysphagia after anterior cervical spine surgery: a review. Global Spine J. 2013;3(4):273-86.
- Three or more levels fused (instead of the more common one or two)3Anderson KK, Arnold PM. Oropharyngeal Dysphagia after anterior cervical spine surgery: a review. Global Spine J. 2013;3(4):273-86.
- Fusion located higher in the cervical spine (above C4)4Mehra S, Heineman TE, Cammisa FP, Girardi FP, Sama AA, Kutler DI. Factors predictive of voice and swallowing outcomes after anterior approaches to the cervical spine. Otolaryngol Head Neck Surg. 2014;150(2):259-65.
- Female gender3Anderson KK, Arnold PM. Oropharyngeal Dysphagia after anterior cervical spine surgery: a review. Global Spine J. 2013;3(4):273-86.
It should also be noted that the experience of the surgeons and types of equipment used likely varied significantly among studies, which could explain why the medical literature has reported conflicting findings on risk factors. There is also some evidence that patients who have an artificial disc replacement instead of a fusion may have less risk for developing dysphagia, but more studies are needed.1Yang Y, Ma L, Liu H et al. Comparison of the incidence of patient-reported postoperative dysphagia between ACDF with a traditional anterior plate and artificial cervical disc replacement. Clinical Neurology and Neurosurgery. 2016; 148: 72-78.
How ACDF Might Cause Dysphagia
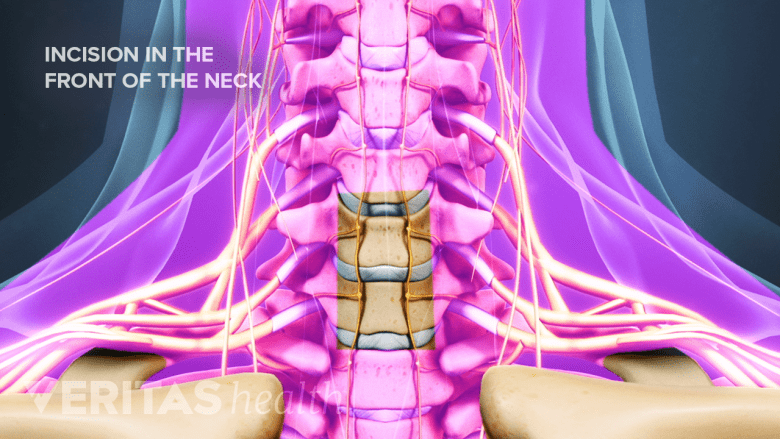
Tissue retraction in the front of the neck carries a potential risk of tissue damage.
The exact cause of dysphagia following ACDF surgery is usually not known. Several different factors could be involved, and most cases resolve before a diagnosis is sought.
Some possible ways that an ACDF surgery could cause dysphagia include:
- Retraction. During ACDF surgery the esophagus and other soft tissues are retracted (pushed to the side) in order to access the cervical spine from the front. While these structures are put back in place after the cervical disc is removed and the bone graft is set up, this shifting and stretching of soft tissues typically results in a sore throat for at least a couple days and potentially contributes to dysphagia.
- Mechanical irritation. Any type of obstruction that pushes up against a structure involved in swallowing, such as the esophagus or a nerve, could cause dysphagia. For example, there have been reports of hardware (placed for fusion) being suspected of contributing to dysphagia.
- Surgical technique. While rare, a surgeon may accidentally nick a structure, such as the esophagus or a nerve, which could potentially lead to a diminished ability to swallow.
See Potential Causes for Dysphagia
Post-ACDF dysphagia usually improves over time but can be a lasting side effect in a small percentage of patients.
When to See the Doctor
If the ability to swallow seems to be getting weaker or if swallowing water is hard or impossible, a doctor should be consulted. Waiting too long to see the doctor could increase the risk of choking.
- 1 Yang Y, Ma L, Liu H et al. Comparison of the incidence of patient-reported postoperative dysphagia between ACDF with a traditional anterior plate and artificial cervical disc replacement. Clinical Neurology and Neurosurgery. 2016; 148: 72-78.
- 2 Yue WM, Brodner W, Highland TR. Persistent swallowing and voice problems after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year follow-up study. Eur Spine J. 2005;14(7):677-82.
- 3 Anderson KK, Arnold PM. Oropharyngeal Dysphagia after anterior cervical spine surgery: a review. Global Spine J. 2013;3(4):273-86.
- 4 Mehra S, Heineman TE, Cammisa FP, Girardi FP, Sama AA, Kutler DI. Factors predictive of voice and swallowing outcomes after anterior approaches to the cervical spine. Otolaryngol Head Neck Surg. 2014;150(2):259-65.

