Here are ideas for evidence-informed gift ideas that support the spine, reduce strain, and improve comfort throughout the day.
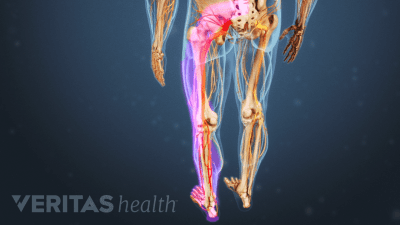
Explore the physiological and mechanical reasons for sciatic pain to flare in the morning – as well as tips on how to address the causes.
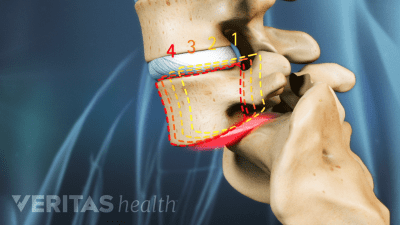
Spinal cord and/or spinal nerve compression occurs when pressure is applied to the spinal cord or and/or nerves, which can causes multiple symptoms.
When you’re considering having spine surgery, complete and reliable information will go a long way in helping you.
What does the term "spondy" actually mean, and why are there so many similar-sounding spine conditions?
Why does this type of nerve pain intensify when you’re trying to sleep, and more importantly how can you calm the pain? Here are 5 insights.
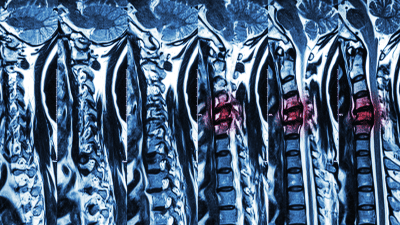
Magnetic resonance imaging (MRI) is a powerful diagnostic tool used to evaluate spine pathology.
For many people, sleeping on your back is one of the best ways to reduce pressure on the spine and promote overnight healing.
Learn about 6 options to help manage your back pain – any one of these could change the way you think about your treatment options.
Walk through 5 common (and costly) mistakes that can delay healing, increase pain, or even lead to long-term damage.