Treatment for painful degenerative disc disease focuses on minimizing pain, stabilizing the spine, and improving or maintaining mobility.
Degenerative disc disease can usually be treated with a combination of pain management techniques, physical therapy, and other approaches.
In This Article:
- Lumbar Degenerative Disc Disease (DDD)
- Lumbar Degenerative Disc Disease Symptoms
- Causes and Risk Factors of Lumbar Degenerative Disc Disease
- Diagnosing Lumbar Degenerative Disc Disease
- Lumbar Degenerative Disc Disease Treatment
- Surgery for Lumbar Degenerative Disc Disease
- Lumbar Degenerative Disc Disease Video
Common Lumbar DDD Treatments
Initial pain management methods for degenerative disc pain typically include a combination of the following:
Over-the-counter (OTC) pain medications
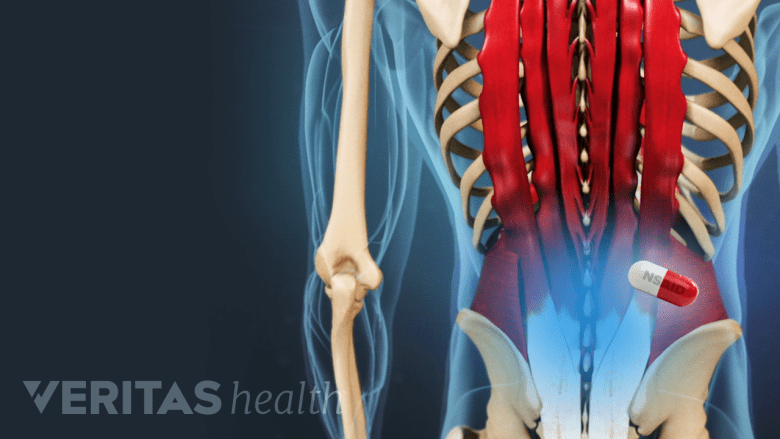
NSAIDs provide anti-inflammatory effects and help calm inflammation and pain in the back.
Aspirin (Bayer), ibuprofen (Advil), or naproxen (Aleve) are common pain medications that can relieve inflammation that contributes to discomfort, stiffness, and nerve root irritation. Acetaminophen (Tylenol) is a pain reliever that interferes with pain signals sent to the brain.
Prescription pain medications
Severe pain that is not relieved with OTC medications may be muscle relaxants or narcotic painkillers. These medications are commonly used to treat intense, acute pain that is not expected to last more than a few days or weeks. These medications can be addictive and cause serious side effects, so they must be used with caution and according to instructions provided by the prescribing doctor.
Heat and ice
The heat pack boosts circulation, reduces spasms, and enhances mobility.
Applying heat to the low back improves circulation, which reduces muscle spasms and tension and improves mobility. Ice packs can reduce inflammation and numb mild pain. It can be helpful to apply heat before physical activities to relax the muscles, and to apply ice after activity to minimize inflammation.
Manual manipulation
Commonly associated with chiropractic care, manual manipulation is a popular pain management method for low back pain. Practitioners use their hands to apply force and pressure to the back, hips, or other areas, with the goal of reducing tension in the muscles and joints. Manual manipulation has been found to be an effective measure for temporarily decreasing pain, and in some cases is as effective as medication.
Massage therapy
Massage therapy can reduce tension and spasms in the low back muscles, reducing pressure on the spine and alleviating pain. Additionally, massage therapy can improve circulation, providing healing nutrients and oxygen to tense muscles.
Epidural steroid injections (ESIs)
A steroid injection administered in the space surrounding the spine can reduce pain signals as well as inflammation. A steroid injection may be used in combination with a physical therapy program to provide pain relief during exercise and rehabilitation. When effective, an epidural steroid injection may alleviate pain for a couple weeks up to one year.
See Epidural Steroid Injection Pain Relief Success Rates
In many cases a combination of treatments is needed for effective pain management. A process of trial and error is typically necessary to find the treatments that best provide meaningful pain relief.
Prolonged bed rest is not recommended, and typically makes back pain worse. It may be helpful to rest for a day or so when pain is most severe, but staying inactive for prolonged periods can weaken the muscles and stiffen the spine, leading to increased pain.
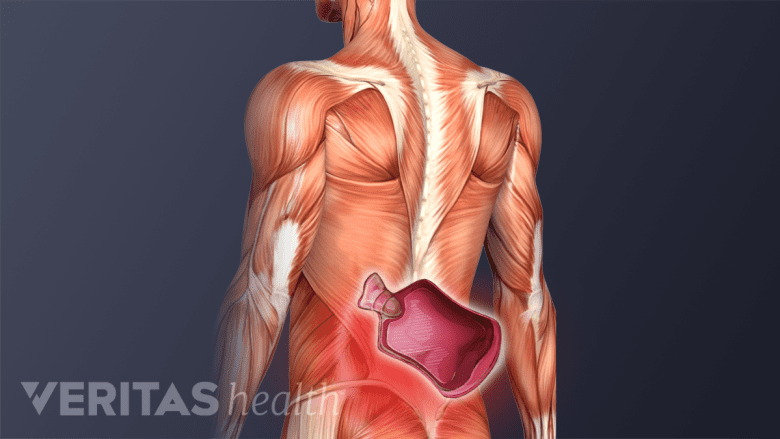
Physical Therapy and Activity Modification
Hamstring stretches promote flexibility and reduce muscle tightness in the lower back and legs.
Physical therapy is often suggested or prescribed to help maintain healthy mobility in the spine. A thorough low back exercise program should include a combination of:
Exercise and Physical Therapy
- Stretching exercises for muscles in the low back, hips, and pelvis, as well as the hamstring muscles. Tightness in these muscles places more pressure on the lumbar spine and contributes to low back pain.
- Strengthening exercises that build lower back and abdominal muscles to maintain healthy postures and better support the spine. Strengthening exercise programs might include a customized physical therapy program, dynamic lumbar stabilization, tai chi, Pilates, or others.
- Low-impact aerobic exercise that elevates the heart rate to improve circulation and deliver nutrients and oxygen necessary for healing the body’s tissues. Examples of aerobics that are gentle on the spine include walking, swimming and water aerobics, stationary biking, and running on an elliptical.
Watch Exercise and Stretching for Lumbar Degenerative Disc Disease Pain Relief Video
Physical therapy programs are usually tailored on a case-by-case basis according to overall health, severity of pain, and personal preferences.
Additionally, making small adjustments to everyday activities (lifestyle modifications) can effectively mitigate pain. For example, wearing a back brace while lifting, or avoiding twisting while lifting, can prevent pain from flaring up due to overuse. Using an ergonomic chair and supportive mattress can also provide daily relief.
Editor’s Top Picks

