The shape and curvature of the spine constantly change through childhood, and these changes can make the spine prone to injury, trauma, and medical conditions.1Ryder C, Harrison K, Johnson K. Back pain in children and adolescents. Paediatrics and Child Health. 2015;25(12):549-554.
The vertebra, which is the bony building block of the spine, predominantly changes from a flexible cartilaginous tissue into the bony skeleton of an adult. Children are unique in terms of their bony skeleton as there are specific areas of the skeleton, known as “growth plates,” where growth occurs. These growth plates are present at the end of each vertebral body and are susceptible to different types of medical problems.1Ryder C, Harrison K, Johnson K. Back pain in children and adolescents. Paediatrics and Child Health. 2015;25(12):549-554.,2Day G, Frawley K, Phillips G, et al. The vertebral body growth plate in scoliosis: a primary disturbance of growth? Scoliosis. 2008;3(1):3. Available from https://scoliosisjournal.biomedcentral.com/articles/10.1186/1748-7161-3-3
As kids age and their bodies mature, it is also possible that an injury to the spinal discs may occur and cause back pain.
In This Article:
- Back Pain in Kids and Teens
- Potential Causes of Back Pain in Children and Teens
- Diagnosing Back Pain in Kids and Teens
- Back Pain Treatment in Kids and Teens
Muscular Pain

Adolescents who participate in sports are at a higher risk for spondylolysis.
The most common cause of back pain in children and adolescents is mechanical pain caused by an injury to one or more groups of muscles in the back.1Ryder C, Harrison K, Johnson K. Back pain in children and adolescents. Paediatrics and Child Health. 2015;25(12):549-554.
Symptoms of muscular back pain in children and adolescents
Classic symptoms and signs of muscular back pain in children and teens typically include1Ryder C, Harrison K, Johnson K. Back pain in children and adolescents. Paediatrics and Child Health. 2015;25(12):549-554.:
- Pain exacerbated by activity or movement
- Pain exacerbated by prolonged sitting or standing
- Pain and tenderness in the muscles on the right and/or left sides of the spine–and not the spine itself
Muscular back pain may be acute, sharp, and stabbing; or chronic, dull, and achy depending on the degree of muscle injury.
Possible causes of muscular back pain in children and adolescents
There may be a history of precipitating trauma, but more often, muscular back pain in children may develop gradually over time and flare insidiously, occurring due to one or a combination of the following factors1Ryder C, Harrison K, Johnson K. Back pain in children and adolescents. Paediatrics and Child Health. 2015;25(12):549-554.:
- Injury while playing or participating in sports
- Carrying a backpack on one shoulder or using excessively heavy backpacks on a regular basis
- Using unsupported posture while sitting, standing, and/or walking
- Sleeping on an overly soft mattress
- Leg length discrepancy
- Obesity
Muscular back pain that develops over time can become chronic and worsen, and may affect the harmony of the surrounding spinal structures if the muscles become weak.
See Back Muscles and Low Back Pain
Spinal Deformity or Malalignment
The growing spinal elements may develop deformities due to external stresses or unexplained causes. Two conditions are discussed below.
Scheuermann's disease
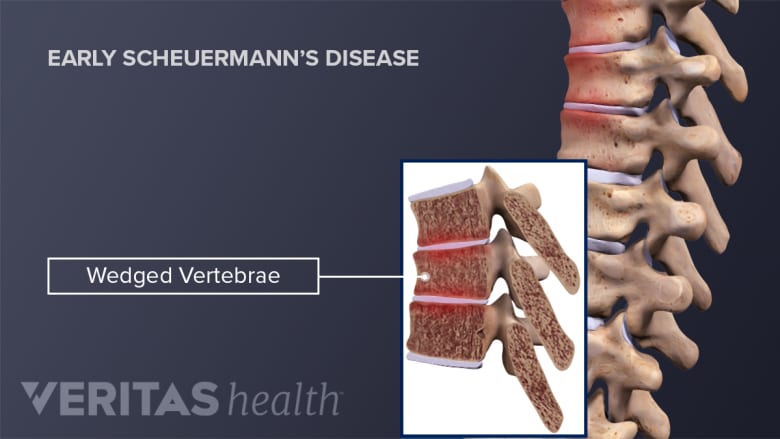
In Scheuermann's disease, the vertebrae are wedge-shaped instead of cylindrical.
In Scheuermann's disease, an abnormality causes parts of the vertebrae to grow at different rates during a child’s growth spurt, causing some vertebrae to become wedge-shaped. These changes result in an exaggerated forward curvature of the upper back, termed “Scheuermann’s kyphosis.”3Mansfield JT, Bennett M. Scheuermann Disease. [Updated 2021 Nov 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan. Available from https://www.ncbi.nlm.nih.gov/books/NBK499966/
The condition manifests around the early- to mid-teenage years and typically causes3Mansfield JT, Bennett M. Scheuermann Disease. [Updated 2021 Nov 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan. Available from https://www.ncbi.nlm.nih.gov/books/NBK499966/:
- Chronic pain in the upper back
- Flaring of pain with activity and improvement with rest
The exact cause of Scheuermann's disease is unknown, but limited evidence suggests that there may be a genetic and/or metabolic component involved.3Mansfield JT, Bennett M. Scheuermann Disease. [Updated 2021 Nov 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan. Available from https://www.ncbi.nlm.nih.gov/books/NBK499966/
See Scheuermann's Disease of the Thoracic and Lumbar Spine
Spondylolysis
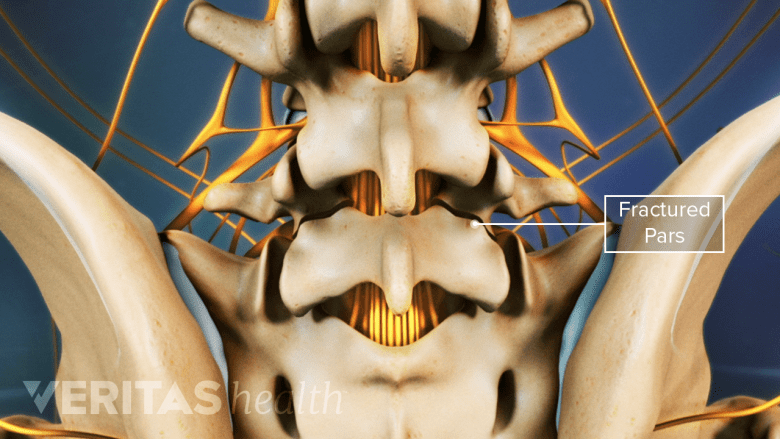
Spondylolysis, a defect in the vertebra’s pars interarticularis, usually occurs at the L5-S1 spinal level.
Athletic adolescents may be at risk of developing spondylolysis, a defect in the pars interarticularis (the joint between the vertebral bones) due to repeated hyperextension (bending backward) and rotation of the spine. Research suggests that this condition mainly affects boys, and up to 50% of adolescent athletes with lower back pain may have this condition.1Ryder C, Harrison K, Johnson K. Back pain in children and adolescents. Paediatrics and Child Health. 2015;25(12):549-554.
The symptoms and signs of spondylolysis may mimic and be mistaken for muscular back pain and can be differentiated and diagnosed by radiologic tests.1Ryder C, Harrison K, Johnson K. Back pain in children and adolescents. Paediatrics and Child Health. 2015;25(12):549-554.
Occasionally, spondylolysis may worsen and progress into spondylolisthesis, the “slipping" of a vertebra upon the one below it. This condition can progress through adolescence.
See Spondylolysis and Spondylolisthesis
Herniated or Injured Spinal Discs
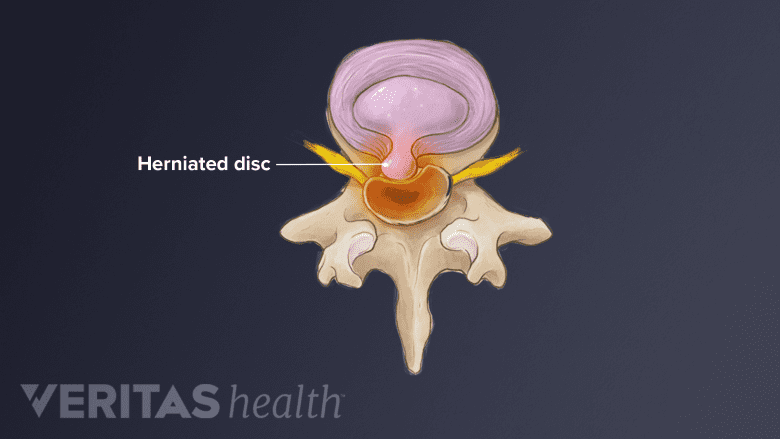
A herniated disc causes nerve root compression and pain along the path of the nerve.
The delicate spinal discs (the spine’s shock absorbers, positioned between each bony vertebra) in children and adolescents may bulge or herniate from acute trauma, such as a fall or motor vehicle accident.
Symptoms of a herniated disc in children and adolescents
A herniated disc in children and adolescents is similar to that in adults and may be associated with sciatica—pain, numbness, and/or weakness radiating down one or both legs, pain while coughing or sneezing (Valsalva maneuver), and/or stiffness in the lower spine.4Bernstein RM, Cozen H. Evaluation of back pain in children and adolescents. AFP. 2007;76(11):1669-1676. Available from https://www.aafp.org/afp/2007/1201/p1669.html
See What's a Herniated Disc, Pinched Nerve, Bulging Disc...?
Discitis
Discitis is a type of infection that affects the spinal disc. Infections affecting the spine are uncommon in children but are serious problems and must be evaluated and treated promptly.1Ryder C, Harrison K, Johnson K. Back pain in children and adolescents. Paediatrics and Child Health. 2015;25(12):549-554.
Discitis predominantly affects younger children between 3 years and 5 years of age. The cause of discitis remains unclear, and researchers believe it may be caused by bacterial or viral infections.1Ryder C, Harrison K, Johnson K. Back pain in children and adolescents. Paediatrics and Child Health. 2015;25(12):549-554.
Symptoms of discitis in children and adolescents
Discitis often occurs insidiously and can cause the following symptoms and signs1Ryder C, Harrison K, Johnson K. Back pain in children and adolescents. Paediatrics and Child Health. 2015;25(12):549-554.:
- Refusal to sit, crawl, or stand
- Abdominal pain and vomiting
- Pain in the hip
- Mild fever
The child may demonstrate relief of symptoms upon lifting under the armpits, thereby relieving pressure on the affected disc.1Ryder C, Harrison K, Johnson K. Back pain in children and adolescents. Paediatrics and Child Health. 2015;25(12):549-554.
Other rare spinal infections that may affect children include vertebral osteomyelitis, spinal TB (Pott’s disease), and epidural abscess.1Ryder C, Harrison K, Johnson K. Back pain in children and adolescents. Paediatrics and Child Health. 2015;25(12):549-554.
Spinal Tumors and Cancer
Benign and malignant tumors of the spine may develop within the spinal cord, from the vertebral bone, due to infiltration of cancer cells in the bone marrow, or from the surrounding nervous tissue.1Ryder C, Harrison K, Johnson K. Back pain in children and adolescents. Paediatrics and Child Health. 2015;25(12):549-554.
Symptoms of spinal tumors and cancer in children and adolescents
Back pain at night that wakes the child from sleep is the hallmark of a spinal tumor. It must, however, be understood that not all children who wake up from sleep due to pain have a spinal tumor. Night-time back pain is especially rare in children below 5 years of age, and this symptom warrants immediate medical attention.1Ryder C, Harrison K, Johnson K. Back pain in children and adolescents. Paediatrics and Child Health. 2015;25(12):549-554.
Spinal tumors and cancers also cause generalized, unexplained weight loss; loss of appetite; and a general feeling of malaise.
Juvenile Ankylosing Spondylitis
Juvenile ankylosing spondylitis is a type of arthritis that causes inflammation of the spine and large joints, resulting in stiffness and pain in the affected areas. The thoracolumbar junction, where the upper back connects with the lower back, and the cervical spine (neck) are the commonly involved parts of the spine.5Burgos-Vargas R., Gutiérrez-Suárez R. (2012) Juvenile Ankylosing Spondylitis. In: Elzouki A.Y., Harfi H.A., Nazer H.M., Stapleton F.B., Oh W., Whitley R.J. (eds) Textbook of Clinical Pediatrics. Springer, Berlin, Heidelberg. Available from https://doi.org/10.1007/978-3-642-02202-9_155
The condition manifests around 6 years to 12 years of age and usually affects boys before puberty and girls after puberty. A genetic predisposition is thought to be the primary cause of juvenile ankylosing spondylitis, and some researchers have also noted bacterial infections and developmental factors to contribute to its evolution.5Burgos-Vargas R., Gutiérrez-Suárez R. (2012) Juvenile Ankylosing Spondylitis. In: Elzouki A.Y., Harfi H.A., Nazer H.M., Stapleton F.B., Oh W., Whitley R.J. (eds) Textbook of Clinical Pediatrics. Springer, Berlin, Heidelberg. Available from https://doi.org/10.1007/978-3-642-02202-9_155
Symptoms of juvenile ankylosing spondylitis in children and adolescents
The onset of this condition causes pain and stiffness in the lower limbs, including the knees, ankles, and feet.5Burgos-Vargas R., Gutiérrez-Suárez R. (2012) Juvenile Ankylosing Spondylitis. In: Elzouki A.Y., Harfi H.A., Nazer H.M., Stapleton F.B., Oh W., Whitley R.J. (eds) Textbook of Clinical Pediatrics. Springer, Berlin, Heidelberg. Available from https://doi.org/10.1007/978-3-642-02202-9_155 As the condition progresses, the spine gets involved and some combination of the following symptoms and signs may be experienced5Burgos-Vargas R., Gutiérrez-Suárez R. (2012) Juvenile Ankylosing Spondylitis. In: Elzouki A.Y., Harfi H.A., Nazer H.M., Stapleton F.B., Oh W., Whitley R.J. (eds) Textbook of Clinical Pediatrics. Springer, Berlin, Heidelberg. Available from https://doi.org/10.1007/978-3-642-02202-9_155:
- Back pain at night that may cause the child to awaken from sleep, especially during the second half of the night
- Morning stiffness of the spine that lasts for 30 minutes or more
- Reduced spinal movement while bending forward and/or sideways
- Pain usually improves after exercise and does not improve with rest
In the later stages, alternating pain may occur in the buttock, hip, and chest areas.5Burgos-Vargas R., Gutiérrez-Suárez R. (2012) Juvenile Ankylosing Spondylitis. In: Elzouki A.Y., Harfi H.A., Nazer H.M., Stapleton F.B., Oh W., Whitley R.J. (eds) Textbook of Clinical Pediatrics. Springer, Berlin, Heidelberg. Available from https://doi.org/10.1007/978-3-642-02202-9_155
Read more about Ankylosing Spondylitis
Scoliosis

Adolescent scoliosis is usually asymptomatic.
While scoliosis (abnormal curvature of the spine) is not an uncommon diagnosis among teenagers, adolescent scoliosis will rarely cause back pain. Teens with scoliosis may develop back pain from other causes, but it has not been found that people with adolescent idiopathic scoliosis are any more likely to develop back pain than the rest of the population.
See Scoliosis: Symptoms, Treatment and Surgery
Tethered Cord Syndrome
Tethered cord syndrome refers to the abnormal attachment of the spinal cord to the tissues that surround it.6Agarwalla PK, Dunn IF, Scott RM, Smith ER. Tethered cord syndrome. Neurosurgery Clinics of North America. 2007;18(3):531-547. DOI: 10.1016/j.nec.2007.04.001 The abnormal attachment results in restriction of normal movement of the spinal cord and/or compromised blood flow to its terminal structures. This spinal condition can be present at birth (congenital) or acquired due to infection, scarring, or tumors affecting the lower back.6Agarwalla PK, Dunn IF, Scott RM, Smith ER. Tethered cord syndrome. Neurosurgery Clinics of North America. 2007;18(3):531-547. DOI: 10.1016/j.nec.2007.04.001
Symptoms of tethered cord syndrome in children and adolescents
Tethering of the spinal cord typically occurs around the lumbosacral junction (L5-S1 spinal segment).6Agarwalla PK, Dunn IF, Scott RM, Smith ER. Tethered cord syndrome. Neurosurgery Clinics of North America. 2007;18(3):531-547. DOI: 10.1016/j.nec.2007.04.001 The symptoms and signs usually depend on the underlying cause of the tethered cord and may change with age.
- Infants may have spontaneous leg movement, abnormal reflexes, foot asymmetry, and thinning of muscle mass in the leg (leg atrophy).6Agarwalla PK, Dunn IF, Scott RM, Smith ER. Tethered cord syndrome. Neurosurgery Clinics of North America. 2007;18(3):531-547. DOI: 10.1016/j.nec.2007.04.001
- Toddlers may exhibit a delay in reaching the walking milestone or may have an abnormal gait.6Agarwalla PK, Dunn IF, Scott RM, Smith ER. Tethered cord syndrome. Neurosurgery Clinics of North America. 2007;18(3):531-547. DOI: 10.1016/j.nec.2007.04.001
- School-age children may have back and leg pain that is often worsened with bending the spine forward (flexion) or vigorous physical activity, sensory deficits and weakness in the legs, painless foot burns (trophic ulcerations), and musculoskeletal deformities of the feet and spine, such as clubfoot or scoliosis.6Agarwalla PK, Dunn IF, Scott RM, Smith ER. Tethered cord syndrome. Neurosurgery Clinics of North America. 2007;18(3):531-547. DOI: 10.1016/j.nec.2007.04.001
- Adolescents typically experience similar symptoms and signs as school-age children with increased sensory deficits, such as bowel and bladder dysfunction and weakness.6Agarwalla PK, Dunn IF, Scott RM, Smith ER. Tethered cord syndrome. Neurosurgery Clinics of North America. 2007;18(3):531-547. DOI: 10.1016/j.nec.2007.04.001
Other common lower back signs of tethered cord syndrome may include pink- or red-colored birthmarks (port-wine stain), swollen fatty nodules (cutaneous lipoma), and deviation of the gluteal crease, among others.6Agarwalla PK, Dunn IF, Scott RM, Smith ER. Tethered cord syndrome. Neurosurgery Clinics of North America. 2007;18(3):531-547. DOI: 10.1016/j.nec.2007.04.001
Psychosocial Factors
Psychosocial factors, such as depression, anxiety, behavioral issues, and pain perception, may be associated with the onset, exacerbation, and/or progress of chronic back pain in children and teens.1Ryder C, Harrison K, Johnson K. Back pain in children and adolescents. Paediatrics and Child Health. 2015;25(12):549-554.,7Prins Y, Crous L, Louw Q. A systematic review of posture and psychosocial factors as contributors to upper quadrant musculoskeletal pain in children and adolescents. Physiotherapy Theory and Practice. 2008;24(4):221-242. DOI: 10.1080/09593980701704089 These factors may also be related to pain in other areas of the spine, such as the neck.7Prins Y, Crous L, Louw Q. A systematic review of posture and psychosocial factors as contributors to upper quadrant musculoskeletal pain in children and adolescents. Physiotherapy Theory and Practice. 2008;24(4):221-242. DOI: 10.1080/09593980701704089
Research suggests that physical pain and psychosocial factors may be linked through neurologic and chemical pathways in the body. Chemicals such as serotonin and norepinephrine that transmit nerve impulses during a physical injury are also known to affect a person’s mood. When there is a dysregulation or imbalance of these chemicals, physical pain may be felt in addition to a psychosocial issue, such as depression, anxiety, or stress.8Trivedi MH. The link between depression and physical symptoms. Prim Care Companion J Clin Psychiatry. 2004;6(Suppl 1):12-16. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC486942/
As a general rule, back pain tends to be relatively uncommon in children and teens and any report of back pain or related worrisome symptoms warrants a consultation with a pediatrician or other qualified healthcare professional.
- 1 Ryder C, Harrison K, Johnson K. Back pain in children and adolescents. Paediatrics and Child Health. 2015;25(12):549-554.
- 2 Day G, Frawley K, Phillips G, et al. The vertebral body growth plate in scoliosis: a primary disturbance of growth? Scoliosis. 2008;3(1):3. Available from https://scoliosisjournal.biomedcentral.com/articles/10.1186/1748-7161-3-3
- 3 Mansfield JT, Bennett M. Scheuermann Disease. [Updated 2021 Nov 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan. Available from https://www.ncbi.nlm.nih.gov/books/NBK499966/
- 4 Bernstein RM, Cozen H. Evaluation of back pain in children and adolescents. AFP. 2007;76(11):1669-1676. Available from https://www.aafp.org/afp/2007/1201/p1669.html
- 5 Burgos-Vargas R., Gutiérrez-Suárez R. (2012) Juvenile Ankylosing Spondylitis. In: Elzouki A.Y., Harfi H.A., Nazer H.M., Stapleton F.B., Oh W., Whitley R.J. (eds) Textbook of Clinical Pediatrics. Springer, Berlin, Heidelberg. Available from https://doi.org/10.1007/978-3-642-02202-9_155
- 6 Agarwalla PK, Dunn IF, Scott RM, Smith ER. Tethered cord syndrome. Neurosurgery Clinics of North America. 2007;18(3):531-547. DOI: 10.1016/j.nec.2007.04.001
- 7 Prins Y, Crous L, Louw Q. A systematic review of posture and psychosocial factors as contributors to upper quadrant musculoskeletal pain in children and adolescents. Physiotherapy Theory and Practice. 2008;24(4):221-242. DOI: 10.1080/09593980701704089
- 8 Trivedi MH. The link between depression and physical symptoms. Prim Care Companion J Clin Psychiatry. 2004;6(Suppl 1):12-16. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC486942/

