Most neck pain can be treated with nonsurgical methods, and there is a wide range of potential treatment options. Many people find effective pain relief through a combination of treatments.
Physical Therapy
Most treatment plans for persistent neck pain include some form of physical therapy to improve neck strength and flexibility. Multiple sessions per week with a trained physical therapist may be recommended to start. After learning the prescribed exercises, you will be instructed to continue the exercise program at home.
Watch 3 Easy Neck Exercises for Neck Pain Video
Medications
Over-the-counter (OTC) pain relief medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen, are typically tried for neck pain.
For severe neck pain, a doctor may prescribe stronger medications for one or two weeks, such as muscle relaxants or opioids.
All medications carry significant potential risks and side effects, even over-the-counter medications such as ibuprofen and acetaminophen, so be sure to work with your doctor and pharmacist.
In This Article:
- All About Neck Pain
- Neck Pain Symptoms
- Neck Pain Causes
- Treatment for Neck Pain
- Surgery for Neck Pain
- Neck Pain Causes Video
Massage therapy
A targeted massage kneads the neck and shoulder muscles with the goal of loosening overly tight muscles that pull on your cervical spine and nerves. A secondary benefit is that massage promotes blood flow to the area, and the blood brings with it healing nutrients. There is not much conclusive evidence that massage is effective for neck pain, but it is low risk and non-invasive and many people find it helps at least in the short term.1Anita R Gross, Haejung Lee, Jeanette Ezzo, Nejin Chacko, Geoffrey Gelley, Mario Forget, Annie Morien, Nadine Graham, Pasqualina L Santaguida, Maureen Rice, Craig Dixon. Massage for neck pain https://pubmed.ncbi.nlm.nih.gov/38415786/. 2024 Feb 28;2(2):CD004871
See Massage Therapy for Chronic Stiff Neck
Manual Manipulation
A chiropractor, osteopath, or other health professional may use their hands to adjust the cervical spine for improved range of motion and reduced pain. Spinal manipulation may be done with a mobilization technique that is slow and gentle, or a a high-velocity manipulation. Manual manipulation is sometimes used to treat certain types of neck pain, depending on the patient’s individual condition and preferences.2Gert Bronfort, Mitchell Haas, Roni L Evans, Lex M Bouter. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis https://pubmed.ncbi.nlm.nih.gov/15125860/. 2004 May-Jun;4(3):335-56.
Acupuncture
A certified acupuncturist places thin needles into specific points on the skin based on the pain type and/or suspected cause. When treating neck pain, the needles may be placed in the neck and/or elsewhere on the body with the goal of unblocking stagnant energy (qi) to promote healing.3Marc A Childress, Samantha Jayne Stuek. Neck Pain: Initial Evaluation and Management https://pubmed.ncbi.nlm.nih.gov/32735440/. 2020 Aug 1;102(3):150-156.
Neck Brace / Cervical Collar
Some people feel better if their neck is supported by a soft cervical collar or brace. For a trauma, such as whiplash, a hard brace or cervical collar may be prescribed. There is mixed evidence about the effectiveness of neck bracing and support, but it is noninvasive and for short periods many people and doctors find it helps reduce pain.4Stefan Muzin, Zacharia Isaac, Joseph Walker, Omar El Abd, Jennifer Baima. When should a cervical collar be used to treat neck pain? https://pmc.ncbi.nlm.nih.gov/articles/PMC2684205/. 2007 Dec 12;1(2):114–119.
Therapeutic Injection Procedures

A cervical epidural steroid injection may provide pain relief by reducing inflammation.
For severe pain that has not gotten better with the most common treatments, a cervical injection may be recommended, for example:
- Cervical epidural. An epidural steroid injection injects a cortisone steroid solution directly into the outer layer of the spinal canal. The goal is to reduce inflammation of nearby nerve roots and tissues.
- Radiofrequency ablation. This procedure may be recommended to treat pain from a facet joint problem. The radiofrequency ablation is designed to interrupt pain signals from reaching the brain by creating a heat lesion at the source.
- Trigger point injection. These injections are usually done using a very thin needle, such as an acupuncture needle. In some cases, a trigger point injection includes a very small amount of local anesthetic to calm an irritated muscle bundle or trigger point.
Injections tend to provide temporary relief because they reduce inflammation or block pain, rather than address the underlying cause.
Watch Cervical Epidural Steroid Injection Video
While the risk is relatively low, injections carry the risk for serious side effects. Injections are typically one of the last treatments to try before considering surgery.
Self-Care for Neck Pain
In addition to medical treatments, most patients engage in their recovery process through self-care techniques and lifestyle modifications, such as:
Short Period of Rest
One or two days of rest can provide a good healing environment. To rest your neck, keep your neck and head in an aligned and supported position.
- Ideally, sleep on your back with a supportive cushion under your neck and a relatively flat pillow to support the natural curves of your cervical spine.
- Some people find use of a soft neck brace for a few days will also help rest the neck during everyday activities.
After a short period of a few hours or days, you will typically be encouraged to gently stretch and move to make sure your neck doesn’t become weaker and stiffer.
Ice and/or Heat
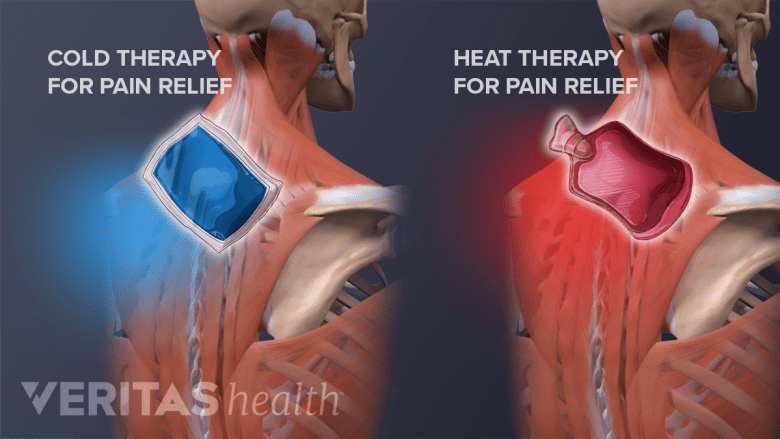
Ice and heat therapy are effective self-care treatments for neck pain.
Simple and inexpensive ice and/or heat therapy is surprisingly effective in reducing neck pain and inflammation.
- Applying ice helps reduce swelling and pain.
- Applying heat helps relax muscles and bring more blood flow and healing nutrients to the injured area.
For ice or heat therapy, applications are limited to 15 or 20 minutes with at least a 2-hour break in between to give the skin time to recover. Some people find continuous application of low-level heat works best, such as a heat wrap that you put on and wear for 4 to 6 hours during the day.
Gentle Stretches
Some forms of neck pain or muscle tightness are alleviated with gentle range-of-motion neck stretches. If a particular movement or stretch exacerbates pain, stop and try another movement instead.
Watch 3 Gentle Stretches to Prevent Neck Pain Video
Mindfulness Meditation
Practicing mindfulness and meditation helps relax your body, reduce pain, and helps by giving a sense of more control over the pain. Various mindful coping methods for pain management are available, such as controlled breathing exercises and distraction techniques.
Cervical Pillow
A pillow specifically designed to keep your cervical spine aligned while sleeping prevents awkward angles and stresses that worsen pain, stiffness or radiculopathy. Another good option is to use a relatively thin pillow, so your neck is not at an angle while you sleep.
Creams and Gels
There is some evidence that application of a topical cream or gel with pain relieving and / or anti-inflammatory properties can relieve local neck pain, particularly pain related to muscle strain.
Many gels and creams are available over-the-counter that anti-inflammatory agents (e.g. Voltaren for arthritis pain, or lidocaine for muscle strain) and/or natural pain-relieving ingredients, such as ginger, tiger balm, and arnica.5Shu Hu, Gianni Belcaro, Maria R Cesarone. A sport cream (Harpago-Boswellia-ginger-escin) for localized neck/shoulder pain https://pubmed.ncbi.nlm.nih.gov/32880419/. 2021 Apr;112(2):255-260.
Pain Patches
Some are designed to work by interrupting the transmission of pain signals, and other patches have pain relieving ointment on them, such as lidocaine, tiger balm, camphor or menthol that penetrates through the skin. Many find them a good choice because the patch sticks to your neck and you can stay active.
In addition, most actions that are good for your overall health will go a long way in helping reduce your neck pain, such as:
- Regular activity and exercise stimulate healthy blood flow and releases endorphins (natural painkillers in your body). For example, take a daily exercise walk, go to an aquatic therapy class a few times a week
- Avoiding smoking, vaping
- Drink enough water so you stay hydrated (your spinal discs are mainly water)
- Get enough vitamins, minerals and nutrition
- Set up your workspace so that it is ergonomically supportive for your neck, e.g. adjust your computer screen so that it is at eye level
- Get enough restorative sleep to provide a better healing environment for your neck6Francisco M Kovacs, Jesús Seco, Ana Royuela, Sergio Melis. Patients with neck pain are less likely to improve if they experience poor sleep quality: a prospective study in routine practice https://pubmed.ncbi.nlm.nih.gov/26153781/. 2015 Aug;31(8):713-21.
- 1 Anita R Gross, Haejung Lee, Jeanette Ezzo, Nejin Chacko, Geoffrey Gelley, Mario Forget, Annie Morien, Nadine Graham, Pasqualina L Santaguida, Maureen Rice, Craig Dixon. Massage for neck pain https://pubmed.ncbi.nlm.nih.gov/38415786/. 2024 Feb 28;2(2):CD004871
- 2 Gert Bronfort, Mitchell Haas, Roni L Evans, Lex M Bouter. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis https://pubmed.ncbi.nlm.nih.gov/15125860/. 2004 May-Jun;4(3):335-56.
- 3 Marc A Childress, Samantha Jayne Stuek. Neck Pain: Initial Evaluation and Management https://pubmed.ncbi.nlm.nih.gov/32735440/. 2020 Aug 1;102(3):150-156.
- 4 Stefan Muzin, Zacharia Isaac, Joseph Walker, Omar El Abd, Jennifer Baima. When should a cervical collar be used to treat neck pain? https://pmc.ncbi.nlm.nih.gov/articles/PMC2684205/. 2007 Dec 12;1(2):114–119.
- 5 Shu Hu, Gianni Belcaro, Maria R Cesarone. A sport cream (Harpago-Boswellia-ginger-escin) for localized neck/shoulder pain https://pubmed.ncbi.nlm.nih.gov/32880419/. 2021 Apr;112(2):255-260.
- 6 Francisco M Kovacs, Jesús Seco, Ana Royuela, Sergio Melis. Patients with neck pain are less likely to improve if they experience poor sleep quality: a prospective study in routine practice https://pubmed.ncbi.nlm.nih.gov/26153781/. 2015 Aug;31(8):713-21.

