Cervical artificial disc replacement (ADR) surgery is typically not recommended unless the procedure is determined to have a good chance of relieving the chronic neck and/or arm pain.
In This Article:
- Cervical Artificial Disc Replacement Surgery
- Considerations for Cervical Disc Replacement Surgery
- Surgical Procedure for Cervical Disc Replacement
- Recovery from Cervical Artificial Disc Replacement Surgery
- Potential Complications and Risks of Cervical Disc Replacement Surgery
- Cervical Disc Replacement Surgery Video
Who Makes a Good Candidate for Cervical ADR?
Cervical artificial disc replacement surgery may be considered for degenerated disc disease treatment.
Good candidates for cervical artificial disc replacement surgery typically have the following indications:
- Confirmed cervical disc disease. An MRI or CT scan with myelography can show soft tissues—such as discs, nerve roots, and the spinal cord—in addition to bones. If imaging shows degeneration of one or more discs, the next step is to determine if any of the degenerating discs correlate to the pain or other symptoms experienced by the patient.
See Cervical Degenerative Disc Disease Symptoms and Diagnosis
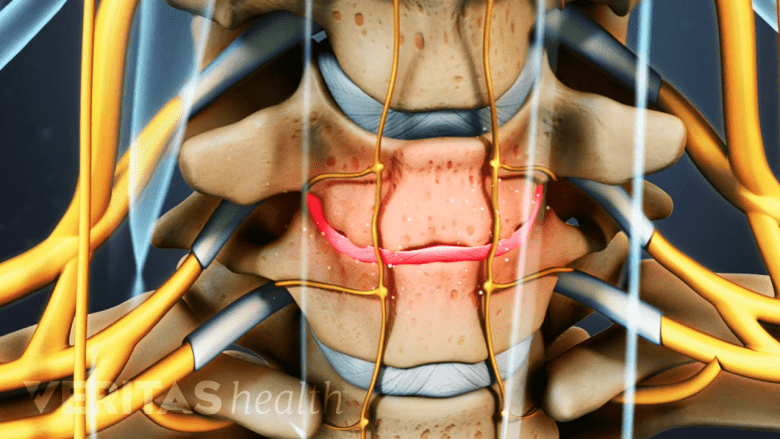
- Radicular pain and/or neurological deficits caused by a problematic disc. Most commonly, an inflamed cervical nerve root corresponds to problems with pain, tingling, numbness, and/or weakness that radiate down into the arm and/or hand. If the spinal cord is compressed within the cervical spine, cervical myelopathic symptoms and/or myelopathy may be experienced anywhere below the level of compression, such as pain that goes into both hands and/or legs, hand weakness/numbness, leg weakness/numbness, trouble with coordination or walking, or difficulty with bladder/bowel control.
- Nonsurgical treatments have been tried. Cervical degenerative disc disease symptoms typically can be managed with nonsurgical treatments, such as rest, ice, heat, medications, physical therapy, and/or therapeutic injections. If the symptoms persist at least 4 to 6 weeks despite nonsurgical treatments, a surgical solution is more likely to be needed for pain relief.1Alentado VJ, Lubelski D, Steinmetz MP, Benzel EC, and Mroz TE. Optimal duration of conservative management prior to surgery for cervical and lumbar radiculopathy: a literature review. Global Spine J. 2014; 4(4):279-86.
- Surgery would be well tolerated. Candidates for cervical ADR must be in generally good health and capable of recovering well from the surgery. The candidate needs to have reached full skeletal maturity (with no more bone growth left) but still be in good enough health for the procedure’s benefits to outweigh the risks. Candidates for cervical ADR are typically between ages 20 and 70.
Even in cases where cervical artificial disc replacement surgery is a viable option, it is almost always up to the patient as to whether to have surgery or not.
Contraindications for Cervical ADR

Artificial discs are not indicated in conditions like facet joint osteoarthritis.
Cervical ADR is not recommended for patients with any of the following:
- Advanced spinal degeneration. Replacing a damaged disc cannot help improve problems associated with an ossified posterior longitudinal ligament or degenerating facet joints, such as from osteoarthritis or ankylosing spondylitis. Also, while artificial cervical discs have been approved for use at 2 adjacent spinal levels by the FDA in some cases, they have not been approved for use in 3 adjacent spinal levels.
- Weakened bones. If the bones are weak, such as from osteoporosis or a bone infection, the artificial disc is less likely to stay in place after the surgery.
- Prior cervical spine surgery. An underlying instability from a previous neck surgery may reduce the chances for cervical ADR to be successful.
- Allergy to artificial disc material. If the patient has a known allergy to any of the metals or plastics in the artificial disc, either a different disc must be selected or the procedure avoided.
Many other potential contraindications exist, such as having a severe spinal deformity or any serious underlying medical condition that would make the surgery and/or the recovery period unlikely to be well tolerated.
- 1 Alentado VJ, Lubelski D, Steinmetz MP, Benzel EC, and Mroz TE. Optimal duration of conservative management prior to surgery for cervical and lumbar radiculopathy: a literature review. Global Spine J. 2014; 4(4):279-86.

