When diagnosing the underlying cause of back pain in kids and teens, a physician will usually evaluate the location of pain and the area(s) of pain distribution. A detailed history of the symptoms, past medical and surgical treatments, and family history is typically discussed with the parents or caregivers.
After a detailed physical exam, the doctor will recommend the necessary radiological and/or laboratory tests to confirm the diagnosis.
In This Article:
- Back Pain in Kids and Teens
- Potential Causes of Back Pain in Children and Teens
- Diagnosing Back Pain in Kids and Teens
- Back Pain Treatment in Kids and Teens
Physical Exam

Physicians typically check the child’s posture and spinal curvatures in a physical exam.
The physical examination of children and adolescents with back pain begins with a visual inspection of the back in a standing posture.1Bernstein RM, Cozen H. Evaluation of back pain in children and adolescents. AFP. 2007;76(11):1669-1676. Available from https://www.aafp.org/afp/2007/1201/p1669.html
Slideshow suggestion:
The physician checks for1Bernstein RM, Cozen H. Evaluation of back pain in children and adolescents. AFP. 2007;76(11):1669-1676. Available from https://www.aafp.org/afp/2007/1201/p1669.html,2Ryder C, Harrison K, Johnson K. Back pain in children and adolescents. Paediatrics and Child Health. 2015;25(12):549-554.:
- Overall posture; spinal symmetry, asymmetry, and/or visual malalignment (such as excessive lumbar lordotic curve or kyphosis)
- Degree of forward and backward bending and any associated pain with these movements
- Ability of the child to touch their toes
- Gait assessment, including the ability to walk on the toes and heels
- Leg length discrepancy
- Color changes of the skin, including cafe au lait patches or freckling
Gently pressing or palpating the back can help the physician evaluate local or generalized tenderness in the back and/or the pelvis.
Clinical Tests
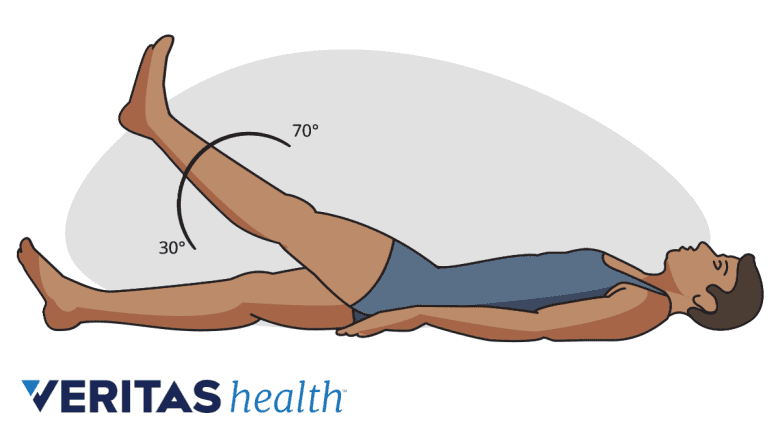
A leg raise test evaluates spinal nerve root irritation, inflammation, or compression.
A thorough motor and sensory examination, including strength testing of specific muscle groups and sensory and reflex testing, is also performed.1Bernstein RM, Cozen H. Evaluation of back pain in children and adolescents. AFP. 2007;76(11):1669-1676. Available from https://www.aafp.org/afp/2007/1201/p1669.html Common tests performed at a physician’s office are2Ryder C, Harrison K, Johnson K. Back pain in children and adolescents. Paediatrics and Child Health. 2015;25(12):549-554.:
- One-legged hyperextension test. This test assesses for spondylolysis. The child is asked to stand on one leg and extend the spine by bending backward. In a positive test, this maneuver results in pain on the same side as the raised leg; for example, if the left leg is raised, pain will occur on the left side of the back.
- Straight leg raise (SLR) test. This test assesses for evidence of spinal nerve root irritation, inflammation, or compression. With the child lying on their back, one leg is gently raised without bending the knee. Pain in the back and/or leg during this test indicates a positive result.
- FABER test. The flexion, abduction, and external rotation (also called FABER) test assesses the sacroiliac (SI) joint. With the patient lying on their back, the physician makes the patient place their leg in a “figure-4” position, where the knee is bent, and the ankle is placed on the opposite knee. A positive test occurs when hip, groin, and/or buttock pain is produced.
The doctor may also test the skin over the lower back and/or leg(s) to check for numbness or loss of sensation, typically seen in conditions that cause nerve root irritation.
Radiographic and Imaging Tests

MRI is useful for detecting tumors, infections, and disc herniation in children and teens.
Depending on the level of concern, one or more of the radiographic and imaging tests described below may be performed.
X-ray
Any suspicion of bone fracture or malalignment warrants an x-ray of the region involved. X-rays do not show soft tissue injuries, such as a muscle pull or a herniated disc, and only the bony components of the spine may be examined.
Computed tomography (CT) scan
If x-ray findings are inconclusive or if more extensive imaging is needed, a CT scan may be ordered. CT scans provide excellent bony detail through multiple views and are also capable of imaging for back pain caused by specific conditions, such as a herniated disc.
See Computerized Tomography (CT) Scan
Magnetic resonance imaging (MRI)
A more advanced type of scan compared to the CT scan is an MRI, which provides in-depth details of bone, joints, muscle, cartilage, and the inner layers of soft tissue surrounding the spine and the spinal cord. MRI is particularly useful for detecting tumors, infections, and disc herniation in children and teens.3Kordi R, Rostami M. Low back pain in children and adolescents: an algorithmic clinical approach. Iran J Pediatr. 2011;21(3):259-270. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3446176/
General anesthesia is usually given to young children who need an MRI.3Kordi R, Rostami M. Low back pain in children and adolescents: an algorithmic clinical approach. Iran J Pediatr. 2011;21(3):259-270. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3446176/
Bone scan
A reasonable alternative to the MRI, a bone scan can help doctors identify bone and soft tissue tumors, and infections.3Kordi R, Rostami M. Low back pain in children and adolescents: an algorithmic clinical approach. Iran J Pediatr. 2011;21(3):259-270. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3446176/
Blood Tests
If an inflammatory condition, infection, or malignancy is suspected, laboratory studies, including complete blood count, erythrocyte sedimentation rate, and C-reactive protein measurement, may be performed.
Once the cause of back pain is determined, a structured treatment approach for the specific condition is formulated. Nonsurgical treatments are usually successful in managing back pain in kids and teens. Rarely, surgery may be needed to treat medical emergencies and specific types of fractures, tumors, or spinal deformity problems.
- 1 Bernstein RM, Cozen H. Evaluation of back pain in children and adolescents. AFP. 2007;76(11):1669-1676. Available from https://www.aafp.org/afp/2007/1201/p1669.html
- 2 Ryder C, Harrison K, Johnson K. Back pain in children and adolescents. Paediatrics and Child Health. 2015;25(12):549-554.
- 3 Kordi R, Rostami M. Low back pain in children and adolescents: an algorithmic clinical approach. Iran J Pediatr. 2011;21(3):259-270. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3446176/

