Degenerative disc disease most commonly occurs in the cervical spine (neck) or the lumbar spine (lower back), as these areas of the spine undergo the most motion and are most susceptible to wear and tear.
In This Article:
The most indicative symptom of degenerative disc disease is a low-grade, continuous pain around the degenerating disc that occasionally flares up into more severe, potentially disabling pain.
See How a Disc Becomes Painful
Pain flare-ups can be related to recent activity and abnormal stress on the spine, or they may arise suddenly with no obvious cause. Episodes can last between a few days to several weeks before returning to low levels of pain or temporarily going away entirely.
Additional Symptoms of Degenerative Disc Disease
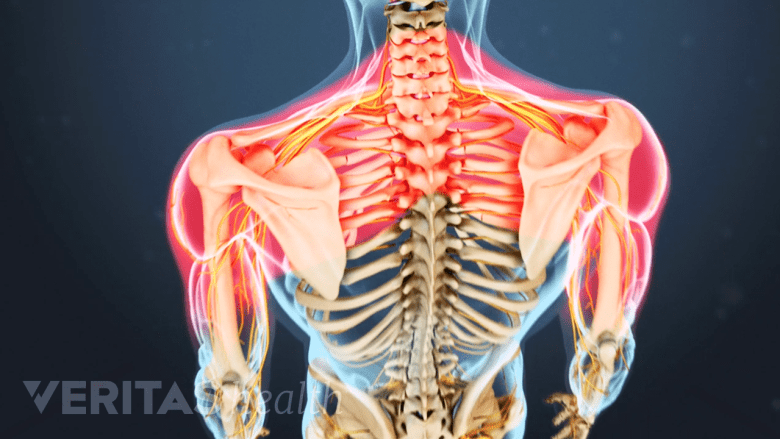
Symptoms of cervical degenerative disc disease include pain in the shoulders, arms, and hands.
Other common symptoms of degenerative disc disease include:
- Increased pain with activities that involve bending or twisting the spine, as well as lifting something heavy
- A “giving out” sensation, caused by spinal instability, in which the neck or back feels as if it is unable to provide basic support, and may lock up and make movement feel difficult.
- Muscle tension or muscle spasms, which are common effects of spinal instability. In some cases, a degenerated disc may cause no pain but muscle spasms are severely painful and temporarily debilitating.
- Possible radiating pain that feels sharp, stabbing, or hot. In cases of cervical disc degeneration, this pain is felt in the shoulder, arm, or hand (called a cervical radiculopathy); in cases of lumbar disc degeneration, pain is felt in the hips, buttocks, or down the back of the leg (called a lumbar radiculopathy).
- Increased pain when holding certain positions, such as sitting or standing for extended periods (exacerbating low back pain), or looking down too long at a cell phone or book (worsening neck pain).
- Reduced pain when changing positions frequently, rather than remaining seated or standing for prolonged periods. Likewise, regularly stretching the neck can decrease cervical disc pain, and taking short, frequent walks during the day can decrease lumbar disc pain.
- Decreased pain with certain positions, such as sitting in a reclining position or lying down with a pillow under the knees, or using a pillow that maintains the neck’s natural curvature during sleep.
The amount of chronic pain—referred to as the baseline pain—is quite variable between individuals and can range from almost no pain or just a nagging level of irritation, to severe and disabling pain.
Chronic pain from degenerative disc disease that is severe and completely disabling does happen in some cases, but is relatively rare.
Diagnosing Degenerative Disc Disease

Degenerative disc issues, such as a cervical herniated disc, can be spotted on an MRI.
The following process is typically used to diagnose degenerative disc disease:
- A medical history is collected that details current and past symptoms of neck or back pain, including when the pain started, how often pain occurs, where pain is felt, and the severity of pain and its impact on mobility. A medical history may also include information on sleep and dietary habits, exercise and activity level, and how symptoms are eased or worsened by activity or posture.
- A physical exam is conducted, which may include feeling along the spine for abnormalities (palpation), a reflex test, and/or a range of motion test that includes bending the spine forward, backward, or to the side.
- An imaging test may be ordered in some cases to find or confirm disc degeneration in the spinal column. An MRI scan is usually used for suspected disc degeneration, which can show disc dehydration, tears or fissures in the disc, or a herniated disc. A dehydrated disc may be referred to as a dark disc or black disc, because it looks darker on an MRI scan.
It is important to note that the amount of pain does not correlate to the amount of disc degeneration. Severely degenerated discs may not produce much pain at all, and discs with little degeneration can produce severe pain—a handful of studies have found prevalent disc degeneration in people not experiencing any disc pain.1Brinjikji W, Luetmer PH, Comstock B, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015;36(4):811-6.,2Berg L, Hellum C, Gjertsen Ø, Neckelmann G, Johnsen LG, Storheim K, Brox JI, Edie GE, Espeland A; Norwegian Spine Study Group. Do more MRI findings imply worse disability or more intense low back pain? A cross-sectional study of candidates for lumbar disc prosthesis. Skeletal Radiology. 2013 Nov; 42(11): 1593-602.
For this reason, a diagnosis of degenerative disc disease should always rely on a combination of a medical history, a physical exam, and any imaging tests ordered.
As a final note, it is helpful for patients to know that the amount of pain does not correlate to the amount of damage in the spine. Severely degenerated discs may not produce much pain at all, and discs with little degeneration can produce severe pain. What this means for patients is that even if they are experiencing severe pain, it does not necessarily mean that there is something seriously wrong with their spine and does not necessarily mean that they need surgery to repair any damage.
- 1 Brinjikji W, Luetmer PH, Comstock B, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015;36(4):811-6.
- 2 Berg L, Hellum C, Gjertsen Ø, Neckelmann G, Johnsen LG, Storheim K, Brox JI, Edie GE, Espeland A; Norwegian Spine Study Group. Do more MRI findings imply worse disability or more intense low back pain? A cross-sectional study of candidates for lumbar disc prosthesis. Skeletal Radiology. 2013 Nov; 42(11): 1593-602.

