The classic presentation of lumbar spinal stenosis is leg pain that increases while walking, standing, or bending backward.1Genevay S, Atlas SJ. Lumbar spinal stenosis. Best Pract Res Clin Rheumatol. 2010;24(2):253‐265. doi:10.1016/j.berh.2009.11.001,2Ammendolia C. Degenerative lumbar spinal stenosis and its imposters: three case studies. J Can Chiropr Assoc. 2014;58(3):312‐319. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4139768/ The pain is typically relieved in 5 to 10 minutes by sitting down or leaning forward at the waist by resting on a counter, walker, or the handle of a shopping cart.1Genevay S, Atlas SJ. Lumbar spinal stenosis. Best Pract Res Clin Rheumatol. 2010;24(2):253‐265. doi:10.1016/j.berh.2009.11.001,2Ammendolia C. Degenerative lumbar spinal stenosis and its imposters: three case studies. J Can Chiropr Assoc. 2014;58(3):312‐319. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4139768/,3Podnar S, Vodušek DB. Lower urinary tract dysfunction in patients with peripheral nervous system lesions. In: Neurology of Sexual and Bladder Disorders. Elsevier; 2015:203-224. doi:10.1016/b978-0-444-63247-0.00012-2 A slightly bent posture may also be adopted while standing and/or walking to reduce the leg pain.1Genevay S, Atlas SJ. Lumbar spinal stenosis. Best Pract Res Clin Rheumatol. 2010;24(2):253‐265. doi:10.1016/j.berh.2009.11.001
In This Article:
Understanding the Symptoms and Progression of Lumbar Spinal Stenosis
In the initial stages of spinal stenosis, a feeling of discomfort, cramping, and/or achiness may develop in the legs after a long walk or prolonged standing. These symptoms may then resolve after sitting, resting, or bending forward. In this stage, activities such as walking outdoors or at a store may cause symptoms. Over time, the pain may become more severe and occur at frequent intervals or remain constant, resulting in leg pain while walking inside the house/apartment.
The symptoms and signs of lumbar spinal stenosis vary depending on the extent of nerve compression and the type of neural tissue affected. While spinal nerve root compression is usually more common, the spinal cord and/or cauda equina may also be compressed due to spinal stenosis. It is also possible for this condition to produce no symptoms or signs.4Dixit R. Low Back Pain. In: Kelley and Firestein’s Textbook of Rheumatology. Elsevier; 2017:696-716.
Understanding Variations in Neural Compression Based on the Type of Stenosis
Depending on the location of neural compression, there are two general types of spinal stenosis—foraminal stenosis, which affects the spinal nerves, and central canal stenosis, which affects the spinal cord and/or the cauda equina.
Foraminal stenosis
This type of stenosis is more common and affects an intervertebral foramen, a short bony canal through which a spinal nerve exits the spinal cord. The part of the nerve where compression occurs is called the nerve root.
Foraminal stenosis can cause nerve root compression in one or more of the following 3 areas:
- Just before it reaches the intervertebral foramen (lateral recess stenosis)
- Within the intervertebral foramen
- Soon after exiting the intervertebral foramen (far lateral stenosis)
In most cases, the lower lumbar motion segments are prone to degenerative foraminal spinal stenosis.5Jenis LG, An HS. Spine Update: Lumbar Foraminal Stenosis. Spine. 2000;25(3):389-394. doi:10.1097/00007632-200002010-00022
Central canal stenosis
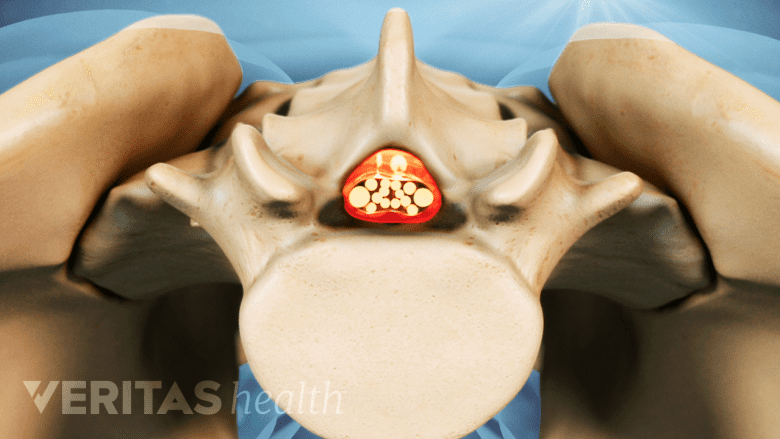
Narrowing of the central canal can compress the spinal cord.
This type of stenosis affects the vertebral foramen—a large opening in the center of the vertebra. The vertebral foramina together form the spinal canal, which houses the spinal cord in the upper lumbar region (L1-L2) and the cauda equina nerves in the middle and lower lumbar regions. When a vertebral foramen narrows, it may compress the spinal cord and/or the cauda equina depending on the location of the affected vertebra.
It is possible for foraminal and central canal stenosis to occur together, causing the symptoms of both conditions to occur.6Patel J, Osburn I, Wanaselja A, Nobles R. Optimal treatment for lumbar spinal stenosis. Current Opinion in Anaesthesiology. 2017;30(5):598-603. doi:10.1097/aco.0000000000000495
Signs and Symptoms of Lumbar Spinal Stenosis: Understanding the Impact on Daily Life

Depending on the cause of lumbar stenosis, the symptoms can vary.
Depending on the type, the signs and symptoms of lumbar spinal stenosis may be localized to specific areas in one leg or affect both legs at the same time. If the sciatic nerve roots are compressed, the symptoms are called sciatica (or radiculopathy) and typically affect the lower back, buttock, thigh, leg, and possibly the foot.
Leg pain caused by spinal stenosis tends to resolve when the spine is bent forward, because this action opens up the narrowed canal, temporarily relieving neural compression.
Lumbar foraminal spinal stenosis symptoms

Nerve pain travels along the spinal nerve into the lower back, thigh, leg, and foot.
Compression of a lumbar spinal nerve as it enters, courses through, or exits the intervertebral foramen may cause some combination of the following symptoms and signs:
- Radicular pain, which originates at the source in the lumbar spine and travels along the path of the affected nerve. Radicular pain is typically characterized by one or more of the following7Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. January 2016:h6234. doi:10.1136/bmj.h6234,8Deasy J. Acquired lumbar spinal stenosis. Journal of the American Academy of Physician Assistants. 2015;28(4):19-23. doi:10.1097/01.jaa.0000462052.47882.fd:
- Sharp, burning, and/or shooting pain in the lower back, thigh, leg, and/or foot
- Dull, aching pain in the lower back, hip, rear pelvis, and/or back and sides of the thigh
- Cramping in the leg and foot
- The pain may occur with prolonged standing or during activities, such as walking or bending the spine backward.9Yamada K, Aota Y, Higashi T, et al. Lumbar foraminal stenosis causes leg pain at rest. Eur Spine J. 2014;23(3):504–507. doi:10.1007/s00586-013-3055-3
Loss of sensation, such as numbness, pins-and-needles, and/or tingling in one or more parts of the thigh, leg, and foot.7Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. January 2016:h6234. doi:10.1136/bmj.h6234,8Deasy J. Acquired lumbar spinal stenosis. Journal of the American Academy of Physician Assistants. 2015;28(4):19-23. doi:10.1097/01.jaa.0000462052.47882.fd
- Weakness of the leg muscles, making it difficult to move the leg and/or foot in different directions.6Patel J, Osburn I, Wanaselja A, Nobles R. Optimal treatment for lumbar spinal stenosis. Current Opinion in Anaesthesiology. 2017;30(5):598-603. doi:10.1097/aco.0000000000000495,7Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. January 2016:h6234. doi:10.1136/bmj.h6234
- Foot drop, which occurs if the L5 spinal nerve root is compressed and results in the inability to lift the front part of the foot.10Stevens F, Weerkamp NJ, Cals JWL. Foot drop. BMJ. 2015;350(apr27 6):h1736-h1736. doi:10.1136/bmj.h1736
- Stiffness in the lower back.8Deasy J. Acquired lumbar spinal stenosis. Journal of the American Academy of Physician Assistants. 2015;28(4):19-23. doi:10.1097/01.jaa.0000462052.47882.fd
Because foraminal spinal stenosis affects a nerve root on either the left or right side of the spine, the symptoms are felt in the left or right leg, along the path of the affected nerve.
Lumbar central canal stenosis symptoms
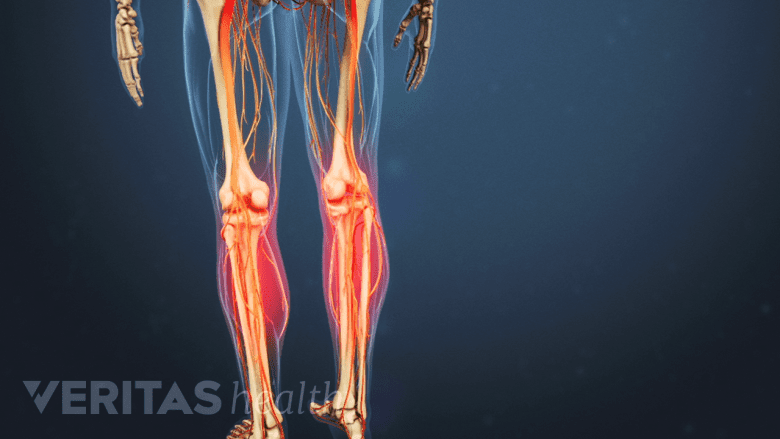
Central canal stenosis can cause burning pain and cramping in the calf area with prolonged standing or walking.
When the spinal cord and/or the cauda equina nerves are compressed due to the narrowing of the internal portion of the vertebral foramen, one or more of the following symptoms may occur, typically following a symmetrical pattern in both legs:
- Neurogenic claudication, a term that describes the set of symptoms characterized by burning pain and cramping in the buttocks, thighs, and calves while standing for long periods of time and/or walking. People experience neurogenic claudication as a feeling of heaviness and tiredness in the legs and difficulty in lifting/moving the legs while walking.
- Abnormal sensation, such as tingling and/or a pins-and-needles feeling in both legs.11Dixit R. Low Back Pain. In: Kelley and Firestein’s Textbook of Rheumatology. Elsevier; 2017:696-716.
- Weakness, resulting in an inability to move or lift the legs.11Dixit R. Low Back Pain. In: Kelley and Firestein’s Textbook of Rheumatology. Elsevier; 2017:696-716.
- Gait problems that typically involve an unsteady, wide-based walking pattern (walking with the legs wide apart).11Dixit R. Low Back Pain. In: Kelley and Firestein’s Textbook of Rheumatology. Elsevier; 2017:696-716.
- Difficulty with balance due to the feeling of not being sure-footed.12Thornes E, Robinson HS, Vøllestad NK. Dynamic balance in patients with degenerative lumbar spinal stenosis; a cross-sectional study. BMC Musculoskelet Disord. 2018;19(1):192. Published 2018 Jun 15. doi:10.1186/s12891-018-2111-x
Read more about Symptoms of Central Canal Stenosis
Progressive compression of the spinal cord or cauda equina can cause conus medullaris syndrome or cauda equina syndrome, resulting in the loss of leg, bowel, and bladder function. Immediate medical attention is required to surgically decompress these neural tissues and prevent permanent nerve damage.
The symptoms of lumbar stenosis may fluctuate, with some periods of more severe symptoms and some with fewer or none. The symptoms may or may not progress over time. The severity and duration of lumbar stenosis symptoms vary between individuals and often dictate whether nonsurgical treatment or spinal surgery is more suitable.
- 1 Genevay S, Atlas SJ. Lumbar spinal stenosis. Best Pract Res Clin Rheumatol. 2010;24(2):253‐265. doi:10.1016/j.berh.2009.11.001
- 2 Ammendolia C. Degenerative lumbar spinal stenosis and its imposters: three case studies. J Can Chiropr Assoc. 2014;58(3):312‐319. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4139768/
- 3 Podnar S, Vodušek DB. Lower urinary tract dysfunction in patients with peripheral nervous system lesions. In: Neurology of Sexual and Bladder Disorders. Elsevier; 2015:203-224. doi:10.1016/b978-0-444-63247-0.00012-2
- 4 Dixit R. Low Back Pain. In: Kelley and Firestein’s Textbook of Rheumatology. Elsevier; 2017:696-716.
- 5 Jenis LG, An HS. Spine Update: Lumbar Foraminal Stenosis. Spine. 2000;25(3):389-394. doi:10.1097/00007632-200002010-00022
- 6 Patel J, Osburn I, Wanaselja A, Nobles R. Optimal treatment for lumbar spinal stenosis. Current Opinion in Anaesthesiology. 2017;30(5):598-603. doi:10.1097/aco.0000000000000495
- 7 Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. January 2016:h6234. doi:10.1136/bmj.h6234
- 8 Deasy J. Acquired lumbar spinal stenosis. Journal of the American Academy of Physician Assistants. 2015;28(4):19-23. doi:10.1097/01.jaa.0000462052.47882.fd
- 9 Yamada K, Aota Y, Higashi T, et al. Lumbar foraminal stenosis causes leg pain at rest. Eur Spine J. 2014;23(3):504–507. doi:10.1007/s00586-013-3055-3
- 10 Stevens F, Weerkamp NJ, Cals JWL. Foot drop. BMJ. 2015;350(apr27 6):h1736-h1736. doi:10.1136/bmj.h1736
- 12 Thornes E, Robinson HS, Vøllestad NK. Dynamic balance in patients with degenerative lumbar spinal stenosis; a cross-sectional study. BMC Musculoskelet Disord. 2018;19(1):192. Published 2018 Jun 15. doi:10.1186/s12891-018-2111-x

