Degenerative spondylolisthesis typically causes low back pain along with a cluster of symptoms and signs in one or both legs.
Degenerative Spondylolisthesis: Common Symptoms and Signs
Degenerative spondylolisthesis symptoms include neurogenic claudication, sciatica, and radiculopathy.
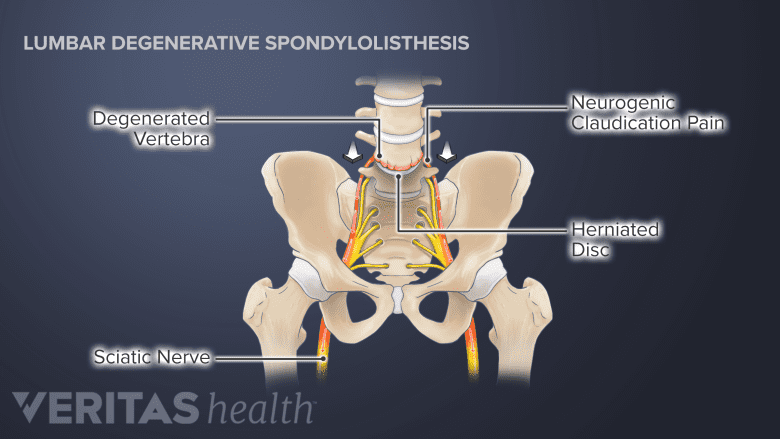
In degenerative spondylolisthesis, the degenerated facet joints and other parts of the vertebral bone tend to increase in size. The enlarged, abnormal bone then encroaches upon the central canal and/or nerve hole (foramen) causing spinal stenosis or foraminal stenosis.
In This Article:
- Degenerative Spondylolisthesis
- Degenerative Spondylolisthesis Symptoms
- Degenerative Spondylolisthesis Treatment
- Surgery for Degenerative Spondylolisthesis
- Degenerative Spondylolisthesis Video
These changes typically result in some combination of the following symptoms and signs.
Persistent low back pain
Low back pain caused by degenerative spondylolisthesis is usually persistent and described as a consistent dull ache,1Cushnie D, Johnstone R, Urquhart JC, Gurr KR, Bailey SI, Bailey CS. Quality of Life and Slip Progression in Degenerative Spondylolisthesis Treated Nonoperatively. Spine (Phila Pa 1976). 2018;43(10):E574-E579. doi:10.1097/BRS.0000000000002429 but it may also feel like a sharp, stabbing sensation for some individuals.
The pain is typically localized in the low back region and may worsen with physical activity, standing, or walking.
Neurogenic claudication
Intermittent neurogenic claudication affects around 75% of people with degenerative spondylolisthesis. It is characterized by episodes of low back pain that radiate to both legs, along with accompanying sensations of tingling, a sensation of weakness, and hamstring spasm.2Li N, Scofield J, Mangham P, Cooper J, Sherman W, Kaye A. Spondylolisthesis. Orthop Rev (Pavia). 2022 Jul 27;14(4):36917. doi: 10.52965/001c.36917. PMID: 35910544; PMCID: PMC9329062.,3García-Ramos CL, Valenzuela-González J, Baeza-Álvarez VB, Rosales-Olivarez LM, Alpizar-Aguirre A, Reyes-Sánchez A. Degenerative spondylolisthesis I: general principles. Espondilolistesis degenerativa lumbar I: principios generales. Acta Ortop Mex. 2020;34(5):324-328..,4Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
It is possible to have any combination of symptoms and they typically occur during walking variable distances or prolonged standing.2Li N, Scofield J, Mangham P, Cooper J, Sherman W, Kaye A. Spondylolisthesis. Orthop Rev (Pavia). 2022 Jul 27;14(4):36917. doi: 10.52965/001c.36917. PMID: 35910544; PMCID: PMC9329062.
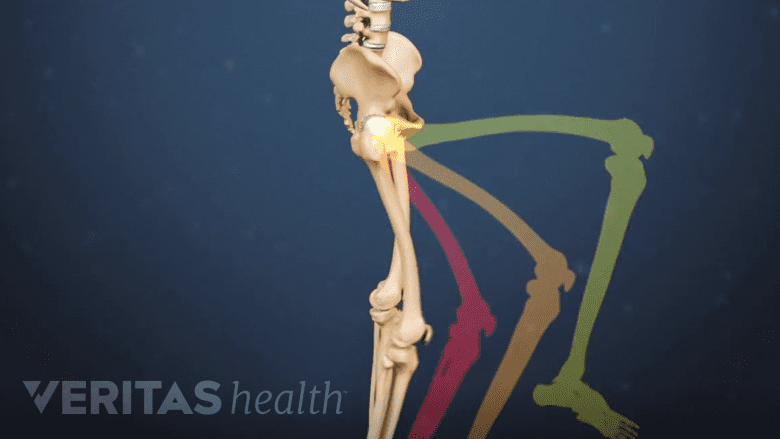
Sciatica: Radiating leg pain
Back pain may radiate into the buttock, thighs, and into the leg and foot.4Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
Radiating leg pain is commonly known as sciatica. This pain occurs due to the irritation, compression, or inflammation of spinal nerve roots in the lower back.4Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
Radiculopathy: Abnormal sensations, weakness, and loss of muscle reflexes
When the spinal nerve roots are compressed or sufficiently inflamed and neurologic deficits are present, the condition is called radiculopathy. Radiculopathy may cause leg weakness and affect muscle reflexes. Additionally, numbness may be felt in the thigh, leg, and/or foot.4Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
It may be challenging to perform activities that require strength, such as walking, climbing stairs, or lifting objects.
Little Known Symptoms of Degenerative Spondylolisthesis
As degenerative spondylolisthesis progresses, the symptoms may lessen due to compensatory mechanisms of the spine that increase spinal stability and prevent further progression.
However, in some individuals, the progression may continue and cause the following symptoms and signs.
Sleep disturbances
Back pain and leg pain may cause disturbed sleep or trouble falling asleep.5Kalichman L, Hunter DJ. Diagnosis and conservative management of degenerative lumbar spondylolisthesis. Eur Spine J. 2008;17(3):327-335. doi:10.1007/s00586-007-0543-3
For this reason, some individuals may choose to sleep in the fetal position (sleeping on the side with knees bent close to the chest) to relieve leg symptoms.5Kalichman L, Hunter DJ. Diagnosis and conservative management of degenerative lumbar spondylolisthesis. Eur Spine J. 2008;17(3):327-335. doi:10.1007/s00586-007-0543-3
Restless leg syndrome
Leg pain and claudication may sometimes cause restless legs syndrome. In this condition, aching or burning pain in the calves causes an irresistible urge to move the legs continuously, causing disturbed sleep.5Kalichman L, Hunter DJ. Diagnosis and conservative management of degenerative lumbar spondylolisthesis. Eur Spine J. 2008;17(3):327-335. doi:10.1007/s00586-007-0543-3
Difficulty walking and imbalance
Degenerative spondylolisthesis may cause difficulty walking and maintaining balance.
As degenerative spondylolisthesis progresses, difficulties with walking and maintaining balance may be experienced. These signs arise from nerve compression caused by the slipped vertebra and associated degenerative changes, Altered posture, muscle weakness and reduced coordination may result.6Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560679/
There are many nerves in our legs that are responsible for relaying information to the brain about position and balance. If these nerves are irritated or compressed in the spine then the brain may not get the necessary information needed for good balance and posture control.
These changes can impact mobility and function, making it harder to engage in normal daily activities.
Limited range of motion
Degenerative spondylolisthesis can affect lumbar range of motion due to the degenerative bone changes that prevent full segmental motion. Muscle spasm and stiffness may result.
Individuals may find it challenging to twist or engage in activities that involve spinal movement. This restricted range of motion can contribute to discomfort and stiffness in the affected area.
Menopause-Related Spondylolisthesis Symptoms
The onset of menopause may accelerate normal degenerative changes of the lumbar vertebrae, discs, facet joints, and ligaments.4Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
Typically, the symptoms associated with this progression include low back pain, stiffness, and/or pain radiating down the leg (sciatica).4Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
Read more about Sciatica Symptoms
Diagnosis of Degenerative Spondylolisthesis
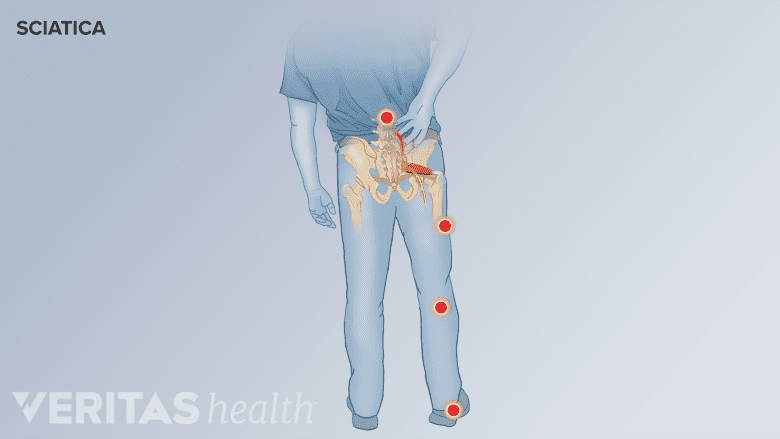
Radiating sciatica pain may occur in degenerative spondylolisthesis.
A physician trained in musculoskeletal conditions can help diagnose degenerative spondylolisthesis.
A comprehensive assessment of the patient’s history, past medical history, thorough physical examination, and review of any prior tests and imaging studies are performed.
During the review of patient history and the physical examination, physicians typically check for7Akkawi I, Zmerly H. Degenerative Spondylolisthesis: A Narrative Review. Acta Biomed. 2022;92(6):e2021313. Published 2022 Jan 19. doi:10.23750/abm.v92i6.10526:
- Pain pattern. Physicians ask about localized or radiating pain and the pattern of pain distribution to check if sciatica is present.
- Postural effects. In degenerative spondylolisthesis, pain is exacerbated while bending backward and relieved when bending forward.
- History of symptoms. Neurogenic claudication and hamstring spasm while walking or standing for variable periods of time may indicate spinal stenosis caused by degenerative spondylolisthesis.
If these symptoms and signs are noticed, the physician may order imaging tests to further investigate the condition.
Imaging Tests for Degenerative Spondylolisthesis
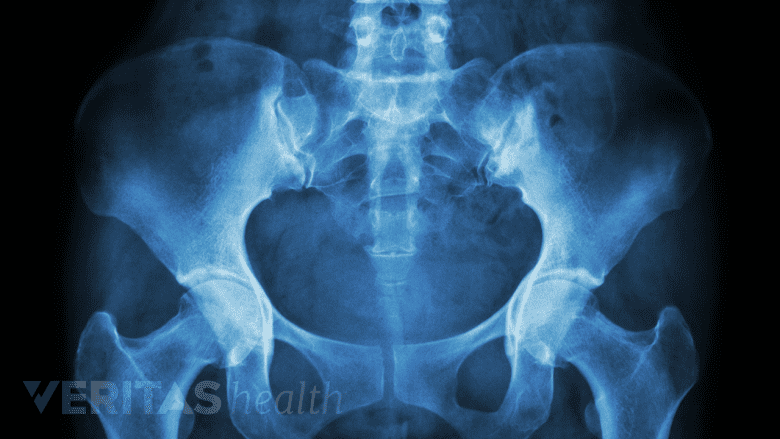
X-rays are helpful in diagnosing and assessing the extent of degenerative spondylolisthesis.
Imaging tests may help confirm the diagnosis of degenerative spondylolisthesis and provide evidence of the extent of progression of the condition.
- Standing lateral radiographs are considered the most reliable and standard test for diagnosing degenerative spondylolisthesis.7Akkawi I, Zmerly H. Degenerative Spondylolisthesis: A Narrative Review. Acta Biomed. 2022;92(6):e2021313. Published 2022 Jan 19. doi:10.23750/abm.v92i6.10526
- Flexion-extension radiographs are used to determine if there is any motion of one vertebra upon the other (translation) and/or instability during spinal movements.7Akkawi I, Zmerly H. Degenerative Spondylolisthesis: A Narrative Review. Acta Biomed. 2022;92(6):e2021313. Published 2022 Jan 19. doi:10.23750/abm.v92i6.10526
- Magnetic resonance imaging (MRI) scans may be used to check for spinal stenosis, nerve root compression, spinal cord involvement, and disc degeneration.3García-Ramos CL, Valenzuela-González J, Baeza-Álvarez VB, Rosales-Olivarez LM, Alpizar-Aguirre A, Reyes-Sánchez A. Degenerative spondylolisthesis I: general principles. Espondilolistesis degenerativa lumbar I: principios generales. Acta Ortop Mex. 2020;34(5):324-328..,7Akkawi I, Zmerly H. Degenerative Spondylolisthesis: A Narrative Review. Acta Biomed. 2022;92(6):e2021313. Published 2022 Jan 19. doi:10.23750/abm.v92i6.10526 Some researchers consider MRI scans as the most reliable test to diagnose spinal stenosis in degenerative lumbar spondylolisthesis.8Matz PG, Meagher RJ, Lamer T, et al. North American Spine Society. Clinical Guidelines for Multidisciplinary Spine Care. Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis. 2nd ed.; 2016.
- CT scans are used if bone involvement such as spondylolysis or isthmic spondylolisthesis is suspected, as these scans provide detailed evaluation of bone integrity.
If an MRI is not possible, computed tomography (CT) scans with myelography may be used as an alternative test.7Akkawi I, Zmerly H. Degenerative Spondylolisthesis: A Narrative Review. Acta Biomed. 2022;92(6):e2021313. Published 2022 Jan 19. doi:10.23750/abm.v92i6.10526,8Matz PG, Meagher RJ, Lamer T, et al. North American Spine Society. Clinical Guidelines for Multidisciplinary Spine Care. Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis. 2nd ed.; 2016.
MRI scans or CT scans may also be used if severe neurogenic claudication is present, bowel and/or bladder incontinence is reported, and/or tumors are suspected.
- 1 Cushnie D, Johnstone R, Urquhart JC, Gurr KR, Bailey SI, Bailey CS. Quality of Life and Slip Progression in Degenerative Spondylolisthesis Treated Nonoperatively. Spine (Phila Pa 1976). 2018;43(10):E574-E579. doi:10.1097/BRS.0000000000002429
- 2 Li N, Scofield J, Mangham P, Cooper J, Sherman W, Kaye A. Spondylolisthesis. Orthop Rev (Pavia). 2022 Jul 27;14(4):36917. doi: 10.52965/001c.36917. PMID: 35910544; PMCID: PMC9329062.
- 3 García-Ramos CL, Valenzuela-González J, Baeza-Álvarez VB, Rosales-Olivarez LM, Alpizar-Aguirre A, Reyes-Sánchez A. Degenerative spondylolisthesis I: general principles. Espondilolistesis degenerativa lumbar I: principios generales. Acta Ortop Mex. 2020;34(5):324-328..
- 4 Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
- 5 Kalichman L, Hunter DJ. Diagnosis and conservative management of degenerative lumbar spondylolisthesis. Eur Spine J. 2008;17(3):327-335. doi:10.1007/s00586-007-0543-3
- 6 Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560679/
- 7 Akkawi I, Zmerly H. Degenerative Spondylolisthesis: A Narrative Review. Acta Biomed. 2022;92(6):e2021313. Published 2022 Jan 19. doi:10.23750/abm.v92i6.10526
- 8 Matz PG, Meagher RJ, Lamer T, et al. North American Spine Society. Clinical Guidelines for Multidisciplinary Spine Care. Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis. 2nd ed.; 2016.

