There are 24 intervertebral discs in the spine. Of those, 12 are located in the thoracic spine. Each thoracic disc sits between two vertebrae to provide cushioning and shock absorption while preventing the vertebrae from grinding against each other.
See Spinal Discs
Thoracic discs tend to be thinner than cervical discs and lumbar discs, which may contribute to the thoracic spine’s relative lack of mobility compared to the neck and lower back. Another distinguishing feature of the thoracic discs is that all but the bottom two interface with ribs.
In This Article:
Thoracic Disc Construction

Thoracic discs act as shock absorbers and prevent the vertebrae from grinding against each other.
Each thoracic disc is comprised of the following:
- Outer layer (annulus fibrosus). This durable exterior of the disc is comprised of tough collagen fibers to help distribute major loads placed on the spine and protect the disc’s soft interior.
- Inner core (nucleus pulposus). This jelly-like interior is a loose network of fibers floating in a mucoprotein gel. The disc’s inner core provides more cushioning and movement between adjacent vertebrae than the outer layer.
Intervertebral discs are the largest structures in the human body that do not have blood vessels. A super-thin structure between the disc and vertebra, called a vertebral end plate, provides diffusion so that nutrients can get into the disc.
How a Thoracic Disc Can Contribute to Pain
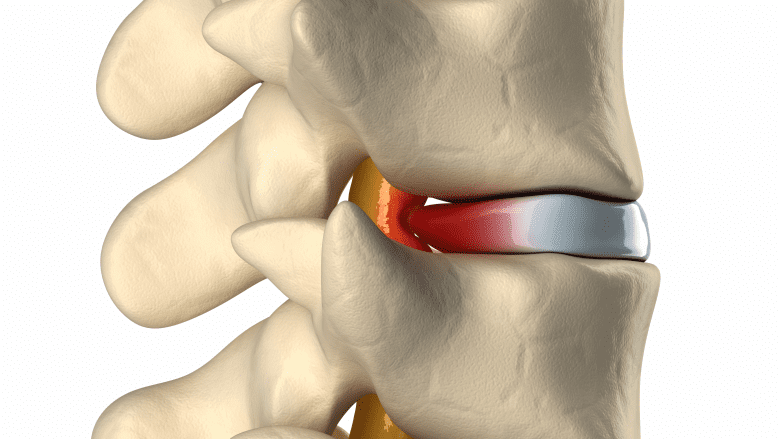
Herniated thoracic discs cause pain by impinging neural tissue.
All intervertebral discs start to lose some hydration as they age and become less flexible. This process of discs drying out and weakening over time is known as degenerative disc disease, but it is typically not diagnosed unless pain or other significant symptoms are present. It is common for degenerative disc disease to progress in conjunction with osteoarthritis.
If degeneration or an injury causes the disc’s outer layer to start developing large enough tears, it is possible for a herniated disc to occur, in which the inner layer leaks outside the disc.
See Thoracic Herniated Disc Causes
In some cases, a herniated disc may inflame a nearby structure, causing pain and/or stiffness. If a nearby thoracic nerve root becomes inflamed, thoracic radiculopathy may occur with symptoms of pain, tingling, numbness, and/or weakness radiating into the chest or abdomen. If the spinal cord becomes inflamed, thoracic myelopathy can occur, which can cause pain, tingling, numbness, and/or weakness to anywhere at that level of the spinal cord or below, as well as the possibility of paralysis and/or the loss of bodily functions, such as bladder or bowel control.
See Thoracic Disc Herniation Symptoms
It is also possible for the disc itself to become painful, such as if a nerve grows deeper into the disc and comes in contact with inflammatory proteins, or if a disc tear involves a sensitive nerve.
Thoracic Disc Pain Is Less Common
Current medical literature indicates that disc degeneration may occur in the thoracic spine about as often as in the more mobile cervical and lumbar spines. However, degenerative disc disease in the thoracic spine is much less likely to cause pain or any other symptoms.
One possibility for this discrepancy may be due to the intervertebral foramen being much bigger in the thoracic spine. While a cervical nerve root takes up about half of the intervertebral foramen and a lumbar nerve root takes up about a third, a thoracic nerve root only takes up about one-twelfth of the foramen, allowing much more room for the spinal nerves and thus reducing the chance that they become pinched or inflamed.1Cramer GD. The thoracic region. In: Cramer GD, Darby SA, ed. Clinical Anatomy of the Spine, Spinal Cord, and ANS. 3rd ed. St. Louise, MO: Elsevier Mosby; 2013:210-245.
- 1 Cramer GD. The thoracic region. In: Cramer GD, Darby SA, ed. Clinical Anatomy of the Spine, Spinal Cord, and ANS. 3rd ed. St. Louise, MO: Elsevier Mosby; 2013:210-245.

