Consultation with a doctor is recommended before using a back brace. A doctor’s evaluation will help determine whether a brace is likely to be beneficial, as well as the type of brace needed and how it should be worn.
It is important to remember that back braces are prescribed as one aspect of a comprehensive treatment program, and that wearing a brace on its own or wearing a brace not according to a doctor’s recommendation may cause further injury and increased pain.
In This Article:
Conditions That Can Benefit from Bracing
In addition to other nonsurgical treatments, a back brace may help heal and relieve pain from the following conditions:
Post-operative healing
A rigid brace may be prescribed following spinal surgery with the goal of reducing pressure on the spinal column, adding stability, and limiting movements and micro-motions to provide a healthy healing environment. A questionnaire completed by spinal surgeons found the most common reason for post-surgical bracing was to limit activity and movement. The same questionnaire showed that back braces were generally recommended between 3 and 8 weeks following surgery, but the duration differed based on a patient’s needs.1Bible JE, Biswas D, Whang PG, Simpson AK, Rechtine GR, Grauer JN. Postoperative bracing after spine surgery for degenerative conditions: a questionnaire study. Spine J. 2009;9(4):309-16.
Isthmic spondylolisthesis

Rigid back braces lessen vertebral slippage and ease pain in isthmic spondylolisthesis.
Using a rigid back brace for isthmic spondylolisthesis has been shown to minimize the amount of vertebral slippage and significantly improve walking ability and pain levels.2Kalichman L, Hunter DJ. Diagnosis and conservative management of degenerative lumbar spondylolisthesis. Eur Spine J. 2008;17(3):327- A rigid brace limits excess motion at the fractured segment, helping control pain and potentially lessening damage to the joints, nerves, and muscles.
Spondylolysis
Similar to isthmic spondylolisthesis, a semi-rigid or rigid brace may be recommended to minimize painful micro-motions at a fractured vertebral level, reducing pain and potentially allowing the fracture to heal. It is thought that a lumbar brace can prevent or reduce vertebral slippage (isthmic spondylolisthesis).
Osteoarthritis

A rigid or semi-rigid back brace reduces instability and painful micro-motions in spinal osteoarthritis.
Instability and painful micro-motions from spinal osteoarthritis may be reduced with the use of a rigid or semi-rigid back brace. Additionally, a brace can reduce pressure on the affected facet joints, alleviating pain and making everyday movements easier, such as moving from a seated to standing position, or vice versa.
Vertebral compression fractures
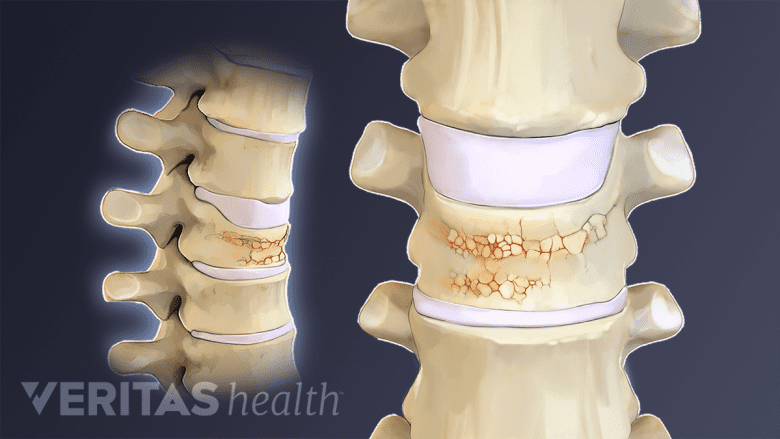
A back brace is used in vertebral compression fractures to minimize micro-motions at the affected level.
A rigid or semi-rigid back brace may be recommended for vertebral compression fractures in order to reduce micro-motions at the fracture or affected vertebral level, as well as reduce pressure on the spinal column.
Degenerative disc disease/lumbar herniated disc
When a spinal disc breaks down and/or herniates, a rigid or semi-rigid back brace can help stabilize and reduce micro-motions at the affected spinal segment. A back brace may also be used to limit bending and twisting and assist in carrying some of the weight the discs normally withstand.
Spinal stenosis
Bracing for lumbar spinal stenosis aims to reduce pressure on and limit micro-motions in the lower spine, both of which can cause nerve root irritation and radicular pain. In some cases, a brace can help adjust posture or shift weight to the abdomen the goal of unloading pressure from the spine.
Muscle tension and strain
A back brace helps alleviate muscle tension by reducing pressure on the spine.
In relatively rare cases, a flexible back brace may be advised for low back muscle strain. A back brace can help alleviate muscle tension by reducing pressure on the spine, thereby reducing the amount of strength needed in the muscles to support the spinal column. Additionally, heat from the brace can help relax tense muscles, contributing to pain relief. A back brace for muscle injury or weakness is generally not recommended for longer than 2 to 4 days.
In some cases a back brace may not be recommended for the above conditions if other treatments are likely to be as or more effective, such as physical therapy, heat or ice application, and/or pain medications.
See Treatment for Lower Back Pain
Back braces have not been shown to help alleviate all low back pain. One study found that patients with specific back pain conditions are more likely to report pain relief after using a back brace than patients with nonspecific back pain.3
Factors for Bracing Success
Some known factors that contribute to bracing success include:
- Wearing the brace as advised. Adherence to wearing a back brace is one of the most important factors for success, although there are many reasons braces may be difficult to wear, such as discomfort or interference in daily activities. If a back brace is too cumbersome or uncomfortable, a doctor can help adjust the brace. It is advised to consult with a doctor before giving up on the brace entirely.
- Viewing a brace as a positive aid. One study found that back bracing provides more effective results when it is thought of as potentially beneficial and a positive attitude is maintained regarding its effects.4Roelofs PD, Van poppel MN, Bierma-zeinstra SM, Van mechelen W. Determinants of the intention for using a lumbar support among home care workers with recurrent low back pain. Eur Spine J. 2010;19(9):1502-7. Encouragement and support from family members, friends, or coworkers can help improve attitudes about a back brace and its ultimate outcomes.
- Not depending on the brace for long-term relief. Back braces are typically recommended on a short-term basis. Wearing a brace longer than recommended is thought to contribute to muscle atrophy and dependence on the brace, which can ultimately weaken the back, increase the chance of injury, and worsen pain.
If a doctor does not think a back brace will be beneficial, it is not recommended to wear one anyway.
- 1 Bible JE, Biswas D, Whang PG, Simpson AK, Rechtine GR, Grauer JN. Postoperative bracing after spine surgery for degenerative conditions: a questionnaire study. Spine J. 2009;9(4):309-16.
- 2 Kalichman L, Hunter DJ. Diagnosis and conservative management of degenerative lumbar spondylolisthesis. Eur Spine J. 2008;17(3):327-
- 3
- 4 Roelofs PD, Van poppel MN, Bierma-zeinstra SM, Van mechelen W. Determinants of the intention for using a lumbar support among home care workers with recurrent low back pain. Eur Spine J. 2010;19(9):1502-7.

