A spinal decompression surgery aims to relieve compression and inflammation around a spinal nerve root, but if the decompression does not relieve pressure around the nerve, is performed at a wrong level, or damages the nerve during the procedure, the symptoms may worsen or continue, and the surgery is considered unsuccessful.
In This Article:
Lumbar decompression typically has a high success rate, with over 75% of patients achieving satisfactory outcomes and symptom resolution.1Sunderland G, Foster M, Dheerendra S, Pillay R. Patient-Reported Outcomes Following Lumbar Decompression Surgery: A Review of 2699 Cases. Global Spine J. 2021;11(2):172-179. doi:10.1177/2192568219896541
- In general, patients begin to feel better within three months of the surgery and continue to get better over time.1Sunderland G, Foster M, Dheerendra S, Pillay R. Patient-Reported Outcomes Following Lumbar Decompression Surgery: A Review of 2699 Cases. Global Spine J. 2021;11(2):172-179. doi:10.1177/2192568219896541
- If there has not been any improvement in the pain approximately 3 months after the decompression, then the back surgery can be assumed to be unsuccessful, and additional treatments may be discussed with the physician.
Common lumbar decompression surgeries are discectomy, microdiscectomy, and laminectomy. The goal of lumbar decompression is to relieve the patient’s back pain and other sciatica symptoms immediately after the back surgery.
Common reasons for a failed lumbar decompression surgery are discussed below.
Missed Disc Fragment
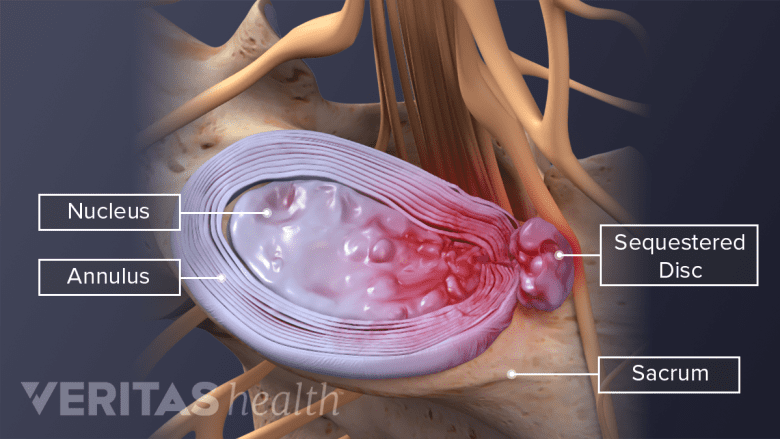
Fragments can migrate away from a herniated disc into the spinal canal space.
When a disc herniates, there’s a 35% to 72% chance that a fragment of the herniated disc will migrate away from the disc and into the spinal canal.2Mallepally AR, Gantaguru A, Marathe N, Meena SK, Tandon V. Missing Disc Fragment: A Rare Surgical Experience. Asian J Neurosurg. 2020;15(3):674-677. Published 2020 Aug 28. doi:10.4103/ajns.AJNS_79_20 These fragments can be identified on imaging tests, such as magnetic resonance imaging (MRI) scans. When a herniated disc is treated with a decompression surgery, the migrated fragments are also removed at the same time. Rarely, surgeons may not be able to locate the migrated fragment during surgery, or it may get missed on the imaging tests and stay in the spinal canal. In such cases, the fragment may affect nearby nerves and cause symptoms in the future.2Mallepally AR, Gantaguru A, Marathe N, Meena SK, Tandon V. Missing Disc Fragment: A Rare Surgical Experience. Asian J Neurosurg. 2020;15(3):674-677. Published 2020 Aug 28. doi:10.4103/ajns.AJNS_79_20
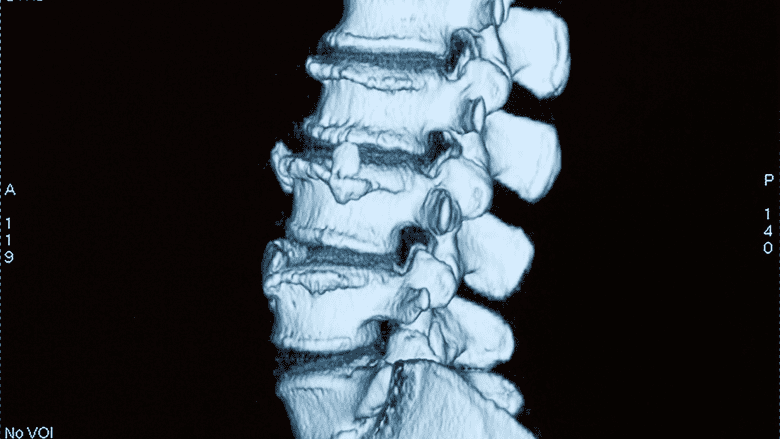
Decompression at the Wrong Level

Surgically treating a wrong spinal level can leave the patient with ongoing symptoms and potentially more pain.
A decompression surgery performed at the wrong level may leave the patient with ongoing symptoms or worsening of symptoms compared to the pre-surgical phase. Uncommon anatomic variations in the patient and failure to follow proper verification protocols by the surgeon are typical causes of wrong-level surgery.3Epstein N. A perspective on wrong level, wrong side, and wrong site spine surgery. Surg Neurol Int. 2021;12:286. Published 2021 Jun 14. doi:10.25259/SNI_402_2021
Research indicates that around 4 to 12 lumbar decompression surgeries per 10,000 surgeries are performed at the wrong spinal level.3Epstein N. A perspective on wrong level, wrong side, and wrong site spine surgery. Surg Neurol Int. 2021;12:286. Published 2021 Jun 14. doi:10.25259/SNI_402_2021
Incorrect Diagnosis
It is essential for the patient's symptoms to match the radiographic test results.
It is not uncommon for a decompression surgery, such as laminectomy, to be performed on a herniated disc that is assumed to be the cause of pain—but actually does not contribute to the patient’s symptoms.4Garcia JB, Rodrigues DP, Leite DR, do Nascimento Câmara S, da Silva Martins K, de Moraes ÉB. Clinical evaluation of the post-laminectomy syndrome in public hospitals in the city of São Luís, Brazil. BMC Res Notes. 2015;8:451. Published 2015 Sep 17. doi:10.1186/s13104-015-1400-9
Decompression surgeries are planned based on imaging test results that show disc herniation, but if the patient’s symptoms and pain do not correlate with the imaging test findings, surgical treatment is not justified.4Garcia JB, Rodrigues DP, Leite DR, do Nascimento Câmara S, da Silva Martins K, de Moraes ÉB. Clinical evaluation of the post-laminectomy syndrome in public hospitals in the city of São Luís, Brazil. BMC Res Notes. 2015;8:451. Published 2015 Sep 17. doi:10.1186/s13104-015-1400-9
Progression of Degeneration

Degeneration of the spinal structures can continue after surgery, leading to long-term symptoms.
Decompression surgery aims to remove the anatomical component that irritates or compresses a nerve root in the spine. Most of these anatomical components arise due to degenerative changes, such as spinal stenosis, osteophytes, or degenerated discs. Surgery removes the specific physical component that obstructs the nerve root but does not address the degenerative process itself. For this reason, it is possible that, in some individuals, degeneration may progress over time and cause the symptoms to occur again.5Mannion AF, Denzler R, Dvorak J, Grob D. Five-year outcome of surgical decompression of the lumbar spine without fusion. Eur Spine J. 2010;19(11):1883-1891. doi:10.1007/s00586-010-1535-2
While this type of symptom recurrence is not due to a failed surgery, doctors advise patients about these potential changes, which can affect the long-term outcome.5Mannion AF, Denzler R, Dvorak J, Grob D. Five-year outcome of surgical decompression of the lumbar spine without fusion. Eur Spine J. 2010;19(11):1883-1891. doi:10.1007/s00586-010-1535-2
Additionally, nerve damage, accumulation of blood or fluids in the surgical site (hematoma/seroma), and wound infection may cause post-surgical complications after a lumbar decompression surgery. Depending on the severity of nerve damage, the symptoms can be transient or permanent.
- 1 Sunderland G, Foster M, Dheerendra S, Pillay R. Patient-Reported Outcomes Following Lumbar Decompression Surgery: A Review of 2699 Cases. Global Spine J. 2021;11(2):172-179. doi:10.1177/2192568219896541
- 2 Mallepally AR, Gantaguru A, Marathe N, Meena SK, Tandon V. Missing Disc Fragment: A Rare Surgical Experience. Asian J Neurosurg. 2020;15(3):674-677. Published 2020 Aug 28. doi:10.4103/ajns.AJNS_79_20
- 3 Epstein N. A perspective on wrong level, wrong side, and wrong site spine surgery. Surg Neurol Int. 2021;12:286. Published 2021 Jun 14. doi:10.25259/SNI_402_2021
- 4 Garcia JB, Rodrigues DP, Leite DR, do Nascimento Câmara S, da Silva Martins K, de Moraes ÉB. Clinical evaluation of the post-laminectomy syndrome in public hospitals in the city of São Luís, Brazil. BMC Res Notes. 2015;8:451. Published 2015 Sep 17. doi:10.1186/s13104-015-1400-9
- 5 Mannion AF, Denzler R, Dvorak J, Grob D. Five-year outcome of surgical decompression of the lumbar spine without fusion. Eur Spine J. 2010;19(11):1883-1891. doi:10.1007/s00586-010-1535-2

