Lumbar laminectomy, also called open decompression, is a surgical procedure performed to treat the symptoms of central spinal stenosis or narrowing of the spinal canal. The surgery involves removal of all or part of the lamina (posterior part of the vertebra) to provide more space for the compressed spinal cord and/or nerve roots.
Lumbar laminectomy is typically considered after nonsurgical treatments such as physical therapy, medications, and/or epidural steroid injections have been tried for a period of 8 to 12 weeks without improvement.1Agabegi SS, McClung HL. Open lumbar laminectomy: Indications, surgical techniques, and outcomes. Seminars in Spine Surgery. 2013;25(4):246-250. doi:10.1053/j.semss.2013.05.004.
Read more about Lumbar Spinal Stenosis Treatment
In This Article:
- Lumbar Laminectomy Surgery for Spinal Stenosis (Open Decompression)
- Considerations for Lumbar Laminectomy (Open Decompression) in Treating Spinal Stenosis
- Surgical Procedure for Lumbar Laminectomy (Open Decompression) in Spinal Stenosis
- Recovery After Lumbar Laminectomy (Open Decompression) for Spinal Stenosis
- Laminectomy and Spinal Stenosis: Risks and Complications
- Lumbar Laminectomy Surgery Video
Goals of Lumbar Laminectomy Surgery
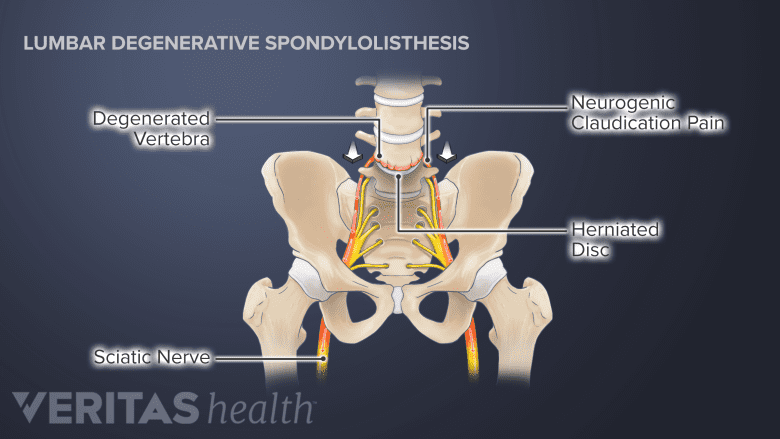
Surgery aims to relieve neural compression and claudication pain from spinal degeneration.
Lumbar laminectomy surgery aims to accomplish the following goals1Agabegi SS, McClung HL. Open lumbar laminectomy: Indications, surgical techniques, and outcomes. Seminars in Spine Surgery. 2013;25(4):246-250. doi:10.1053/j.semss.2013.05.004.:
- Relieve neural tissue compression. Stenosis of the spinal canal in the lumbar region may cause compression of the spinal cord, thecal sac, spinal dura, and/or the cauda equina. When one or more of these structures are compressed, neurogenic claudication (leg pain while walking or bending the spine backward) may occur, typically affecting both legs. Laminectomy helps relieve the compression of these neural tissues by widening the spinal canal.
- Improve leg function. Lumbar stenosis often causes decreased mobility due to pain and weakness in one or both legs. Laminectomy helps decrease pressure on the nerves, reducing leg pain, and potentially improving weakness and functionality of the lower back and legs.
One or more spinal motion levels may be treated together. It is important to note that lumbar laminectomy primarily aims to treat leg symptoms and not lower back pain. Back pain may persist even after the surgery due to pain from the continuing degeneration process or from causes unrelated to nerve or spinal cord compression.1Agabegi SS, McClung HL. Open lumbar laminectomy: Indications, surgical techniques, and outcomes. Seminars in Spine Surgery. 2013;25(4):246-250. doi:10.1053/j.semss.2013.05.004.,2Lee SY, Kim TH, Oh JK, Lee SJ, Park MS. Lumbar Stenosis: A Recent Update by Review of Literature. Asian Spine J. 2015;9(5):818–828. doi:10.4184/asj.2015.9.5.818
Types of Lumbar Laminectomy for Spinal Stenosis
Lumbar laminectomy relieves neural compression by removing the bone compressing the nerve tissue.
Depending on the amount of lamina removed or the technique used to relieve neural compression, a lumbar laminectomy can be of the following types:
- Bilateral laminectomy: Both sides of the lamina of the affected vertebra are removed with or without widening of the intervertebral foramina and/or removal of adjacent tissue and bone.
- Unilateral laminotomy: A part of or the entire lamina on one side of the affected vertebra is removed with or without adjacent tissues.
Unilateral laminotomy may also be performed by using an endoscope (a small tube), which is minimally invasive and requires a smaller incision compared to open surgery. While minimally invasive techniques may preserve more tissue and bone and reduce healing time, the overall success rates of open and minimally invasive decompression are usually the same.3Anilbhai Thaker R, Goda N, Shukla S, Chaddha R. Comparative Study of Unilateral Laminotomy versus Conventional Laminectomy. Global Spine Journal. 2014;4(1_suppl):s-0034-1376742-s-0034-1376742. doi:10.1055/s-0034-1376742.,4Ang C-L, Phak-Boon Tow B, Fook S, et al. Minimally invasive compared with open lumbar laminotomy: no functional benefits at 6 or 24 months after surgery. The Spine Journal. 2015;15(8):1705-1712. doi:10.1016/j.spinee.2013.07.46.
In some lumbar vertebrae, the facets may be partially or completely removed. In such cases, a fusion of the vertebrae is considered to retain stability.
Success Rates of Lumbar Laminectomy for Spinal Stenosis
The success rate of a lumbar laminectomy to alleviate leg pain from spinal stenosis is generally favorable. Research suggests:
- 85% to 90% of lumbar central spinal stenosis patients find relief from leg pain after an open laminectomy surgery.5Dakwar E, Deukmedjian A, Ritter Y, Dain Allred C, Rechtine GR II. Spinal Pathology, Conditions, and Deformities. In: Pathology and Intervention in Musculoskeletal Rehabilitation. Elsevier; 2016:584-611. doi:10.1016/b978-0-323-31072-7.00016-6.
- 75% of patients may have satisfactory outcomes for up to 10 years postoperatively.1Agabegi SS, McClung HL. Open lumbar laminectomy: Indications, surgical techniques, and outcomes. Seminars in Spine Surgery. 2013;25(4):246-250. doi:10.1053/j.semss.2013.05.004.
Although the outcome of lumbar laminectomy is usually good, about 10% to 15% of patients may subsequently require a repeat surgery due to post-operative complications.6Wai EK, Roffey DM, Tricco AC, Dagenais S. Decompression Surgery. In: Evidence-Based Management of Low Back Pain. Elsevier; 2012:403-421. doi:10.1016/b978-0-323-07293-9.00029-5.
Improper diagnosis, physical deconditioning before and/or after surgery, and smoking are a few examples of causes for surgical failure. Choosing the right candidate who may benefit from this surgery can help prevent future complications.
- 1 Agabegi SS, McClung HL. Open lumbar laminectomy: Indications, surgical techniques, and outcomes. Seminars in Spine Surgery. 2013;25(4):246-250. doi:10.1053/j.semss.2013.05.004.
- 2 Lee SY, Kim TH, Oh JK, Lee SJ, Park MS. Lumbar Stenosis: A Recent Update by Review of Literature. Asian Spine J. 2015;9(5):818–828. doi:10.4184/asj.2015.9.5.818
- 3 Anilbhai Thaker R, Goda N, Shukla S, Chaddha R. Comparative Study of Unilateral Laminotomy versus Conventional Laminectomy. Global Spine Journal. 2014;4(1_suppl):s-0034-1376742-s-0034-1376742. doi:10.1055/s-0034-1376742.
- 4 Ang C-L, Phak-Boon Tow B, Fook S, et al. Minimally invasive compared with open lumbar laminotomy: no functional benefits at 6 or 24 months after surgery. The Spine Journal. 2015;15(8):1705-1712. doi:10.1016/j.spinee.2013.07.46.
- 5 Dakwar E, Deukmedjian A, Ritter Y, Dain Allred C, Rechtine GR II. Spinal Pathology, Conditions, and Deformities. In: Pathology and Intervention in Musculoskeletal Rehabilitation. Elsevier; 2016:584-611. doi:10.1016/b978-0-323-31072-7.00016-6.
- 6 Wai EK, Roffey DM, Tricco AC, Dagenais S. Decompression Surgery. In: Evidence-Based Management of Low Back Pain. Elsevier; 2012:403-421. doi:10.1016/b978-0-323-07293-9.00029-5.

