Constipation following spine surgery is common and may occur even if there is no prior history of constipation before the surgical procedure.
Post-surgical constipation often remains unaddressed, leaving patients to endure significant and unnecessary discomfort and pain.
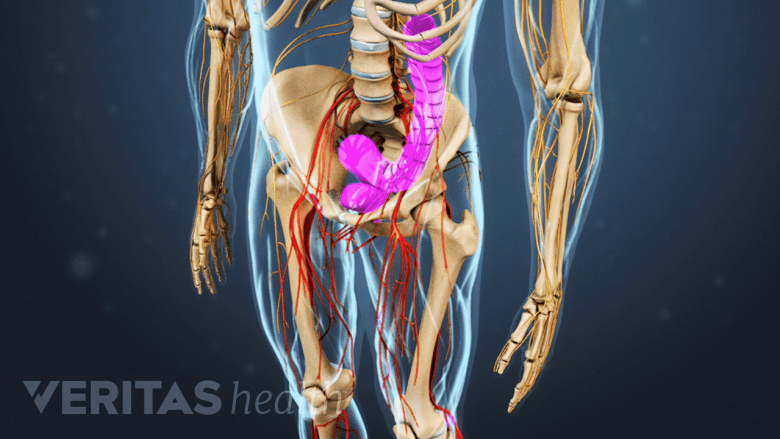
Gastrointestinal issues and constipation are common side effects of back surgery.
In This Article:
- Preventing Constipation After Back Surgery
- Medications for Constipation Relief
How Spine Surgery Causes Constipation
There are many aspects of having back surgery that can contribute to constipation, including:
- Use of anesthesia1Stienen MN, Smoll NR, Hildebrandt G, Schaller K, Tessitore E, Gautschi OP. Constipation after thoraco-lumbar fusion surgery. Clin Neurol Neurosurg. 2014;126:137-142. doi:10.1016/j.clineuro.2014.08.036
- Blood loss during surgery1Stienen MN, Smoll NR, Hildebrandt G, Schaller K, Tessitore E, Gautschi OP. Constipation after thoraco-lumbar fusion surgery. Clin Neurol Neurosurg. 2014;126:137-142. doi:10.1016/j.clineuro.2014.08.036
- Longer duration of surgery1Stienen MN, Smoll NR, Hildebrandt G, Schaller K, Tessitore E, Gautschi OP. Constipation after thoraco-lumbar fusion surgery. Clin Neurol Neurosurg. 2014;126:137-142. doi:10.1016/j.clineuro.2014.08.036
- Use of specific types of pain medications1Stienen MN, Smoll NR, Hildebrandt G, Schaller K, Tessitore E, Gautschi OP. Constipation after thoraco-lumbar fusion surgery. Clin Neurol Neurosurg. 2014;126:137-142. doi:10.1016/j.clineuro.2014.08.036
- Decreased activity levels and increased bed rest1Stienen MN, Smoll NR, Hildebrandt G, Schaller K, Tessitore E, Gautschi OP. Constipation after thoraco-lumbar fusion surgery. Clin Neurol Neurosurg. 2014;126:137-142. doi:10.1016/j.clineuro.2014.08.036
- Increased stress
- Dietary changes
- Decreased mobility or lack of mobility
The use of opioid medication to manage post-surgical pain is one of the most common causes of constipation after surgery, affecting 40% to 90% of patients who take these medications.2Rauck RL, Hong K soo J, North J. Opioid-induced constipation survey in patients with chronic noncancer pain. Pain Pract. 2017;17(3):329-335. doi:10.1111/papr.12445
When Constipation Is Diagnosed
Constipation is diagnosed if fewer than three bowel movements occur in a week in addition to 2 or more of the following criteria3Lammers E, Srivastava SB. Constipation treatment: a review. Orthopaedic Nursing. 2020;39(3):194-198. doi:10.1097/NOR.0000000000000657:
- Straining during a bowel movement
- Lumpy or hard stools
- Sensation of intestinal obstruction while passing stools
- Sensation of incomplete evacuation
- The need for manual maneuvers to aid defecation
Patients may also feel pain in the stomach, rectum, and/or anus with a sensation of bloating and nausea.
Risk Factors for Post-Surgical Constipation
The risk of postsurgical constipation is higher in older men and in lumbar surgical approaches done from the front or side of the body,4Yue JK, Krishnan N, Wang AS, Chung JE, Etemad LL, Manley GT, Tarapore PE. A standardized postoperative bowel regimen protocol after spine surgery. Front Surg. 2023 Mar 17;10:1130223. doi: 10.3389/fsurg.2023.1130223. PMID: 37009608; PMCID: PMC10063852. such as anterior lumbar interbody fusion (ALIF), transforaminal lumbar interbody fusion (TLIF), extreme lateral interbody fusion (XLIF), or anterior-posterior spine surgery.
How Long Post-Surgical Constipation Lasts
Post-surgical constipation may last for several days or weeks and may even extend to months depending on the cause.
As long as opioid medications are used to manage post-surgical pain, the risk of constipation is generally high.
Discussing alternate pain medications with the doctor and taking necessary steps to prevent constipation from developing helps reduce the risk of chronic constipation.
12 Simple Lifestyle Changes to Prevent Constipation After Surgery
Incorporating simple lifestyle adjustments will go a long way in preventing or reducing constipation. The most effective measures to encourage regular bowel movements are discussed below.
1. Get up and walk as soon as possible after surgery
Walking encourages bowel motility and stimulates the digestive system to keep things moving smoothly through the intestines.5Huang R, Ho SY, Lo WS, Lam TH. Physical activity and constipation in Hong Kong adolescents. PLoS One. 2014 Feb 28;9(2):e90193. doi: 10.1371/journal.pone.0090193. PMID: 24587274; PMCID: PMC3938666. Walking also helps the body heal from the effects of spine surgery, enabling a quicker return to daily functions and lesser pain-related disabilities.6Pester BD, Yoon J, Yamin JB, Papianou L, Edwards RR, Meints SM. Let's Get Physical! A Comprehensive Review of Pre- and Post-Surgical Interventions Targeting Physical Activity to Improve Pain and Functional Outcomes in Spine Surgery Patients. J Clin Med. 2023 Mar 30;12(7):2608. doi: 10.3390/jcm12072608. PMID: 37048691; PMCID: PMC10095133.
Early mobilization also helps to reduce complications such as deep vein thrombosis, pneumonia, and infection post-surgery.
It is advisable to start with frequent, short walks throughout the day, gradually extending to longer walks as recommended by the doctor.
2. Engage in physical therapy and stretching to aid bowel movements
Physical movements triggered by exercise have a direct impact on the muscles of the stomach and intestine, promoting the movement of stool through the rectum.7Gao R, Tao Y, Zhou C, et al. Exercise therapy in patients with constipation: a systematic review and meta-analysis of randomized controlled trials. Scandinavian Journal of Gastroenterology. 2019;54(2):169-177. doi:10.1080/00365521.2019.1568544
Exercise also aids in alleviating abdominal distention and bloating caused by constipation.7Gao R, Tao Y, Zhou C, et al. Exercise therapy in patients with constipation: a systematic review and meta-analysis of randomized controlled trials. Scandinavian Journal of Gastroenterology. 2019;54(2):169-177. doi:10.1080/00365521.2019.1568544
Slow walking, brisk walking, gentle stretching, and resistance training exercises as guided by the therapist are examples of simple exercises that can be performed after surgery.
3. Limit the use of opioid pain medications
Most opioid pain medications (eg, Vicodin, Darvocet, Percocet, and Oxycontin) slow bowel motility and cause constipation. As such, limiting the use of these medications to the minimum dosage necessary for adequate pain control will reduce the risk of constipation.
For several patients, non-opioid pain relievers provide significant pain relief, and these drugs do not cause constipation.
Some newer medications that block the effect of opioid receptors in the gut (such as Movantik) are available, but these are usually not readily covered by most insurances.
See Opioid Medication Potential Risks and Complications
4. Use over-the-counter (OTC) laxatives in moderation
While OTC laxatives provide temporary relief from constipation, excessive or prolonged use can lead to dependency and disrupt the natural bowel function. Overuse of laxatives has been linked to dehydration and electrolyte imbalances in some people.8Sato Y, Fukudo S. Gastrointestinal symptoms and disorders in patients with eating disorders. Clin J Gastroenterol. 2015 Oct;8(5):255-63. doi: 10.1007/s12328-015-0611-x. Epub 2015 Oct 26. PMID: 26499370.
If constipation persists, it's best to address the underlying cause rather than relying solely on laxatives.
5. Consider natural laxatives
Natural laxatives are gentle and safe non-drug remedies that help promote regular bowel movements and relieve constipation. Examples of natural laxatives include:
- Fruits like prunes, apples, and kiwis, which are rich in fiber and sorbitol, a natural sugar with laxative properties.
- Vegetables, such as spinach and broccoli, which contain fiber and help regulate bowel movements.
- Seeds, such as flaxseeds and chia seeds, which have laxative properties due to their high fiber and oil content.
- Herbal teas made from senna, dandelion, or peppermint.
Using these remedies early, before the signs and symptoms of constipation develop, can help prevent the condition from developing and maintain a healthy gut.
6. Stay well hydrated
Drinking plenty of fluids (water and non-caffeinated drinks) is essential for maintaining good digestion, keeping the stool soft, and preventing constipation.
It is recommended to drink at least 40 oz of water per day, provided that the physician has not restricted fluid intake for another reason.
7. Consume a fiber-rich diet
Eating foods that are naturally high in fiber helps stimulate the intestines for a bowel movement. Fiber helps sweep away waste, promoting regular bowel movements.
Examples of high-fiber foods include beans, bran cereals, fresh fruits (such as watermelon, grapes, and prunes), and vegetables (such as lettuce and carrots).
8. Limit processed foods
Processed and fast foods often lack the necessary nutrients and fiber required for smooth digestion and may induce constipation if consumed in large amounts. Examples of processed foods are cheese, processed meat, and canned foods.
9. Set a bathroom routine
It’s essential to pay attention to the body’s natural bowel habits. Establishing a regular bathroom routine by visiting the toilet at the same time each day helps regulate bowel movements, reducing the chances of constipation.
10. Don’t ignore the urge to have a bowel movement
Ignoring the urge to have a bowel movement can lead to stool becoming harder and drier, making it difficult to pass later. It's essential to respond promptly to the body's signals and prioritize regular bathroom visits to maintain adequate digestive health.
11. Manage stress
Spine surgery is a stressful event, and chronic stress can affect the digestive system, leading to constipation.9Chang YM, El-Zaatari M, Kao JY. Does stress induce bowel dysfunction? Expert Rev Gastroenterol Hepatol. 2014 Aug;8(6):583-5. doi: 10.1586/17474124.2014.911659. Epub 2014 May 31. PMID: 24881644; PMCID: PMC4249634. Engaging in stress-relieving activities like yoga, meditation, or spending time in nature keeps the stress levels low and bowel movements more regular.
12. Maintain a healthy weight
Being either overweight or underweight can impact digestive health. By adhering to a well-balanced diet and engaging in regular exercise, one can achieve a healthy weight, promoting bodily equilibrium and reducing the risk of constipation.
Every individual is unique, and what works for one person may not work for another. If persistent or severe constipation is experienced despite making lifestyle changes, it is essential to seek medical advice to rule out any underlying health conditions and/or get prescription medications to help relieve constipation.
Potential Complications of Constipation after Spine Surgery
Severe or chronic constipation leads to potential complications after surgery. These complications may include:
- Wound dehiscence. Straining to pass stools can cause a surgical incision to open, leading to wound dehiscence.
- Hemorrhoids. Straining can cause the veins near the anus and lower rectum to swell and bleed, leading to pain and discomfort.
- Anal fissure. Passing large or hard stools can tear the lining of the large intestine near the anus, causing burning pain and bleeding with a bowel movement.
- Fecal impaction. Chronic constipation can cause stool to become stuck in the colon or rectum.
- Rectal prolapse. Straining to pass stool can cause the rectum to stretch and protrude through the anus.
- Post-operative ileus. A condition caused by decreased bowel motility, resulting in abdominal distension, pain, and vomiting.
A revision surgery or additional interventions may be needed to manage these complications if they become severe or cause additional problems.
When to See a Doctor
While occasional or mild constipation is not alarming, certain signs and symptoms warrant medical attention, including:
- Not having a bowel movement for several days
- Severe abdominal pain, bloating, and/or vomiting
- Difficulty or pain while passing gas
- A sudden change in bowel habits after surgery
- Noticing blood in the stool
These symptoms usually indicate underlying complications that require immediate evaluation and treatment.
See When Back Pain May Be a Medical Emergency
Early intervention can help prevent further complications and ensure a smoother healing journey.
- 1 Stienen MN, Smoll NR, Hildebrandt G, Schaller K, Tessitore E, Gautschi OP. Constipation after thoraco-lumbar fusion surgery. Clin Neurol Neurosurg. 2014;126:137-142. doi:10.1016/j.clineuro.2014.08.036
- 2 Rauck RL, Hong K soo J, North J. Opioid-induced constipation survey in patients with chronic noncancer pain. Pain Pract. 2017;17(3):329-335. doi:10.1111/papr.12445
- 3 Lammers E, Srivastava SB. Constipation treatment: a review. Orthopaedic Nursing. 2020;39(3):194-198. doi:10.1097/NOR.0000000000000657
- 4 Yue JK, Krishnan N, Wang AS, Chung JE, Etemad LL, Manley GT, Tarapore PE. A standardized postoperative bowel regimen protocol after spine surgery. Front Surg. 2023 Mar 17;10:1130223. doi: 10.3389/fsurg.2023.1130223. PMID: 37009608; PMCID: PMC10063852.
- 5 Huang R, Ho SY, Lo WS, Lam TH. Physical activity and constipation in Hong Kong adolescents. PLoS One. 2014 Feb 28;9(2):e90193. doi: 10.1371/journal.pone.0090193. PMID: 24587274; PMCID: PMC3938666.
- 6 Pester BD, Yoon J, Yamin JB, Papianou L, Edwards RR, Meints SM. Let's Get Physical! A Comprehensive Review of Pre- and Post-Surgical Interventions Targeting Physical Activity to Improve Pain and Functional Outcomes in Spine Surgery Patients. J Clin Med. 2023 Mar 30;12(7):2608. doi: 10.3390/jcm12072608. PMID: 37048691; PMCID: PMC10095133.
- 7 Gao R, Tao Y, Zhou C, et al. Exercise therapy in patients with constipation: a systematic review and meta-analysis of randomized controlled trials. Scandinavian Journal of Gastroenterology. 2019;54(2):169-177. doi:10.1080/00365521.2019.1568544
- 8 Sato Y, Fukudo S. Gastrointestinal symptoms and disorders in patients with eating disorders. Clin J Gastroenterol. 2015 Oct;8(5):255-63. doi: 10.1007/s12328-015-0611-x. Epub 2015 Oct 26. PMID: 26499370.
- 9 Chang YM, El-Zaatari M, Kao JY. Does stress induce bowel dysfunction? Expert Rev Gastroenterol Hepatol. 2014 Aug;8(6):583-5. doi: 10.1586/17474124.2014.911659. Epub 2014 May 31. PMID: 24881644; PMCID: PMC4249634.

