Spinal fusion surgery for scoliosis is extensive and only recommended when lateral curves are likely to cause severe deformity. It is important for patients to understand the potential complications of surgery.
In This Article:
- Spinal Fusion for Idiopathic Scoliosis
- Scoliosis Surgery: Potential Risks and Complications
Scoliosis Surgery Risks
Scoliosis surgeries today tend to be safer and achieve better outcomes than ever before. However, any surgery—especially a surgery on the spine near the spinal cord—has risks. Scoliosis surgery risks could include:
1. Paraplegia
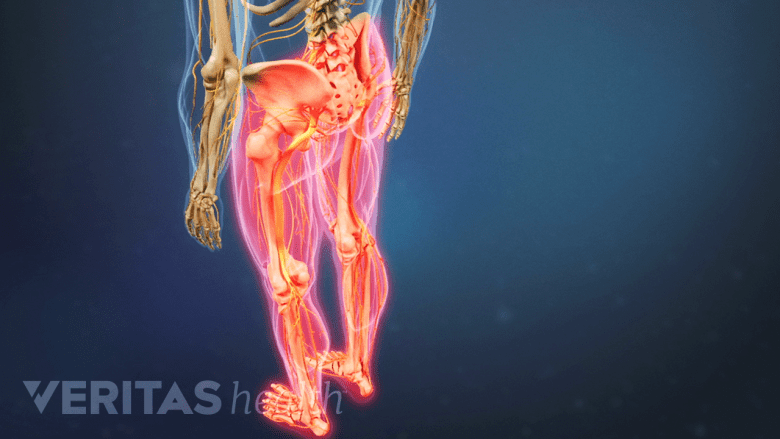
Rarely, scoliosis surgery may lead to loss of sensation and movement in the lower body.
The most concerning risk with scoliosis surgery is paraplegia—loss of movement and feeling in the lower body and legs. It is rare but can be a devastating complication. To help manage this risk, the spinal cord is monitored during surgery through a several simultaneous methods:
- Somatosensory evoked potential (SSEP). This monitoring test involves small electrical impulses that are given in the legs and then read in the brain. These signals should remain constant throughout the surgery. If the signals begin to slow at any point, this can indicate compromise to the spinal cord or its blood supply.
- Motor evoked potential (MEP). This test is similar to SSEP, but MEP instead monitors signals related to muscles. If possible, it is good to use both tests throughout the surgery because in rare cases one test might reveal a spinal cord disturbance that the other test would have missed.
- Stagnara wake-up test. This test involves waking the patient during surgery and asking them to move the feet. The patient does not feel any pain during this procedure and will likely not remember it afterwards. Due to improvements in SSEP and MEP, the wake-up test is rarely used anymore.
See Scoliosis Surgery: Postoperative Care
If any of these aforementioned tests indicates spinal cord compromise, the rods can be removed and the surgery changed. While this situation is rare, it is worth every precaution to prevent potential risk damage to the spinal cord.
By detecting a spinal cord complication when it first starts—such as from too much compression or loss of blood—the surgical team can quickly work to restore as much of the spinal cord’s health as possible.
2. Excessive Blood Loss
There is a lot of muscle stripping and exposed area during the surgery, which leads to blood loss. With proper technique, the blood loss can usually be kept to a reasonable amount and blood transfusions are rarely needed.
As a precaution, the patient may donate his or her own blood prior to surgery (autologous blood donation), which can then be given back to the patient, if needed, after the surgery. Also, during scoliosis surgery the patient's blood can be collected and transfused back to the patient.
3. Other Risks
Other potential complications could include:
- Failure of the spine to fuse (also called pseudoarthosis)
- Infection
- Cerebrospinal fluid leak
- Instrumentation failure (rods breaking or hooks/screws dislodging)
Some surgical complications, such as rods breaking or the spine not fusing, could result in the scoliosis continuing to worsen.
Problems That Can Develop Later

Inflammation or degeneration of adjacent tissues is a potential risk of fusion surgery.
Sometimes structural problems can develop years after the surgery. For example, the discs directly above and below the fusion may be subjected to increased loads due to the inflexibility of the spine between them. It is possible for these discs to degenerate sooner than the normal aging of the spine, which in some cases could result in a second surgery.
Other examples could include:
- Flat-back syndrome. This syndrome is caused by the loss (or flattening) of the natural lordosis curve in the low back and may become a cause of lower back pain. Before surgeons had the ability to do three-dimensional corrections of the spine, the side-to-side curvature of scoliosis got corrected without considering how that might be changing the natural front-to-back curvature. Modern surgical techniques reduce the risk for flat-back syndrome.
- Crankshaft phenomenon. This painful deformity can occur when the front of the spine keeps growing while the back of the spine does not. Before this principle was widely understood, there were times in the past when surgeons would fuse the back of a growing child’s spine without also fusing the front. Surgeons today should know how to do fusions to avoid the crankshaft phenomenon.
- Adding-on phenomenon. There have been cases in which a child or adolescent has a thoracic curve fused, but the curve continues to progress (add on) beneath the fusion level. The adding-on phenomenon is still being studied, but it appears to be more likely if the surgeon does not fuse low enough and/or the patient is still too skeletally immature for a fusion surgery.
Most people who are candidates for scoliosis surgery benefit from spinal fusion. However, as with any surgery, careful consideration should also be given to the potential risks before making a final decision.
Editor’s Top Picks
- Scoliosis Surgery
- Scoliosis Surgery: Planning for Postoperative Care at Home
- Scoliosis Surgery Recovery: At the Hospital (4 to 7 Days)
- Scoliosis Surgery Recovery: After Discharge (First 14 Days)
- Scoliosis Surgery Recovery: After Discharge (2 Weeks to 3 Months)
- Scoliosis Surgery Recovery: 3 Months Post-Operation and Beyond

