Epidural steroid injections are a common treatment for neck and back pain. These injections typically deposit steroids and/or other medications in the epidural space of the spine. The epidural space contains nerves, blood vessels, and fat; and surrounds the dura, a sac around the spinal cord.
Epidural steroid injections may be given in the cervical, thoracic, lumbar or sacral regions of the spine. Prior to the injection, the skin over the treatment site is cleaned and numbed by injecting a local anesthetic.
In This Article:
How Epidural Steroid Injections Work
Epidural steroid injections may be given purely as steroids, purely anesthetic, or steroids mixed with an anesthetic medication and/or saline. These injections work by:
- Controlling the inflammatory response from chemical and mechanical sources of pain such as a pinched nerve or a degenerated disc.
- Reducing the activity of the immune system to decrease the production of inflammatory cells in the body.
The steroids injected into the epidural space disperse into the nerve endings and other tissues, spreading the anti-inflammatory effect throughout the pain-transmitting structures.
Read more about How Epidural Steroid Injections Work
When epidural steroid injections are used
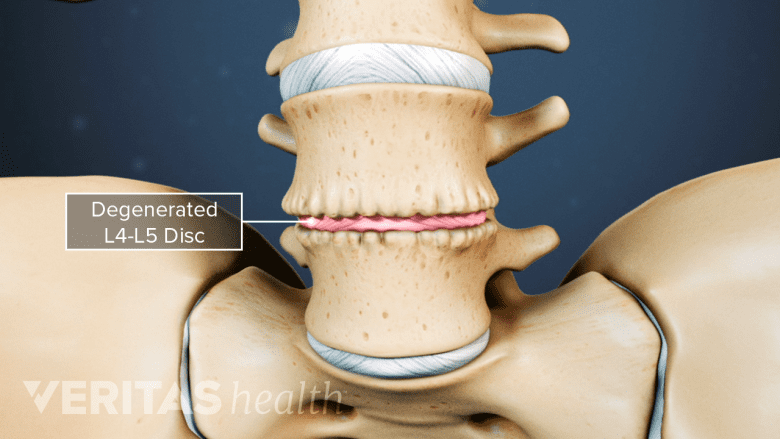
Epidural steroid injections can alleviate pain caused by degenerative disc disease.
Epidural steroid injections may help relieve pain stemming from conditions such as spinal stenosis, foraminal stenosis, disc herniation, or degenerative disc disease. An epidural injection can be given in the neck, mid-back or lower back/buttocks. The injections can be used to treat pain in each of these three regions or pain that radiates out from these areas into the arms and legs and less frequently into the chest/thorax.
Read more about Indications for Lumbar Epidural Injections
How Epidural Steroid Injections are Given

Epidural injections use three routes: interlaminar, transforaminal, and caudal, targeting different areas of the spine.
Different routes or approaches are possible to inject medication into the epidural space.1Manchikanti L, Nampiaparampil DE, Candido KD, et al. Do cervical epidural injections provide long-term relief in neck and upper extremity pain? A systematic review. Pain Physician. 2015;18(1):39-60. These routes include:
- Transforaminal injection—the needle is inserted into the epidural space through the intervertebral foramen on the side of the spinal canal. A space above the spinal nerve as it exits the neuroforamen called the safe triangle is the region where the needle is usually passed to reach the epidural space. This technique is called the supraneural approach.
- Interlaminar injection—the needle is inserted into the space between adjacent vertebral laminae (posterior wall of the vertebra) to reach the epidural space.
- Caudal injection—the needle is placed into the sacral area below the lumbar spine through an opening called the sacral hiatus.
The procedure should always be performed under fluoroscopy (x-ray guidance) with a contrast dye.
See Epidural Injection Procedure
Success Rates of Epidural Steroid Injections
Several studies have proven the efficacy of epidural steroid injections throughout the spine. Studies show that an effective first-response to an epidural steroid injection may be considered as an opportunity to administer more injections when the symptoms return.2Murthy NS, Geske JR, Shelerud RA, et al. The Effectiveness of Repeat Lumbar Transforaminal Epidural Steroid Injections. Pain Medicine. 2014;15(10):1686-1694. doi:10.1111/pme.12497 However, it is important to note that when initial relief is not experienced, additional injections should not be given.
See Epidural Steroid Injection Pain Relief Success Rates
A few clinical findings include:
- In the cervical spine, 54% to 80% of patients reported significant improvement in pain and functional outcome from 6 months to 2 years (with a total of 3 to 6 injections given during this period).1Manchikanti L, Nampiaparampil DE, Candido KD, et al. Do cervical epidural injections provide long-term relief in neck and upper extremity pain? A systematic review. Pain Physician. 2015;18(1):39-60.,3Park KD, Lee WY, Nam SH, Kim M, Park Y. Ultrasound-guided selective nerve root block versus fluoroscopy-guided interlaminar epidural block for the treatment of radicular pain in the lower cervical spine: a retrospective comparative study. Journal of Ultrasound. December 2018. doi:10.1007/s40477-018-0344-z
- In the lumbar spine, 53% to 56% of patients reported significant improvement in pain and functional outcome up to 1 year (a total of 3 to 4 injections were given during this period).4Meng H, Fei Q, Wang B, et al. Epidural injections with or without steroids in managing chronic low back pain secondary to lumbar spinal stenosis: a meta-analysis of 13 randomized controlled trials. Drug Des Devel Ther. 2015;9:4657–4667. Published 2015 Aug 13. doi:10.2147/DDDT.S85524
See Lumbar Epidural Steroid Injections for Low Back Pain and Sciatica
Some patients may, however, experience little to no pain relief.
The effectiveness of epidural steroid injections typically improves when additional therapies, such as physical therapy and therapeutic exercises are used in a prescribed manner. The success of treatment also depends on the accuracy with which the medication is delivered to the pain source.
See Physical Therapy for Low Back Pain Relief and Physical Therapy for Neck Pain Relief
Risks and Complications of Epidural Steroid Injections
Although rare, some serious risks associated with epidural steroid injections include infection, nerve damage, bleeding, dural puncture (cerebrospinal fluid leak), and/or damage to the spinal cord. The risk of neurological complications may be higher in the cervical spine compared to the lumbar spine. Typically, the transforaminal injections carry a higher risk of complications compared to interlaminar or caudal injections.
- 1 Manchikanti L, Nampiaparampil DE, Candido KD, et al. Do cervical epidural injections provide long-term relief in neck and upper extremity pain? A systematic review. Pain Physician. 2015;18(1):39-60.
- 2 Murthy NS, Geske JR, Shelerud RA, et al. The Effectiveness of Repeat Lumbar Transforaminal Epidural Steroid Injections. Pain Medicine. 2014;15(10):1686-1694. doi:10.1111/pme.12497
- 3 Park KD, Lee WY, Nam SH, Kim M, Park Y. Ultrasound-guided selective nerve root block versus fluoroscopy-guided interlaminar epidural block for the treatment of radicular pain in the lower cervical spine: a retrospective comparative study. Journal of Ultrasound. December 2018. doi:10.1007/s40477-018-0344-z
- 4 Meng H, Fei Q, Wang B, et al. Epidural injections with or without steroids in managing chronic low back pain secondary to lumbar spinal stenosis: a meta-analysis of 13 randomized controlled trials. Drug Des Devel Ther. 2015;9:4657–4667. Published 2015 Aug 13. doi:10.2147/DDDT.S85524

