Spinal cord stimulation (SCS) uses mild electric pulses to interrupt pain signals traveling from the spinal cord to the brain. The pulses are generated in a small, implanted device called a spinal cord stimulator and delivered to a rich network of nerves near the spinal cord through thin wires.
This FDA-approved treatment is recommended for select individuals with chronic pain caused by nerve or blood vessel problems.1 It is commonly proposed as a treatment for failed back surgery syndrome (FBSS).
Since spinal cord stimulation acts directly on the nerve tissue and alters nerve activity, it is also called neurostimulation or neuromodulation.
In This Article:
- Spinal Cord Stimulation for Chronic Back and Neck Pain
- Who May Benefit from Spinal Cord Stimulation
- Spinal Cord Stimulation: The Trial Period
- Spinal Cord Stimulator Implantation Surgery: Step by Step
- Disadvantages and Risks of Spinal Cord Stimulation
- Spinal Cord Stimulation for Chronic Back Pain Video
- Spinal Cord Stimulation for Chronic Neck Pain Video
4-Step Process of Spinal Cord Stimulation Treatment
Individuals considering spinal cord stimulation typically follow these steps:
Step 1: Consultation
A physician evaluates the patient to determine if the underlying cause of pain can be addressed through spinal cord stimulation treatment.
Step 2: Testing
Diagnostic tests are ordered, and a mental health evaluation is performed. These tests include but are not limited to:
- Radiographic tests, such as magnetic resonance imaging (MRI) or computed tomography (CT), to evaluate the space around the spinal cord in the mid and/or lower back, where the treatment wires will be inserted
- Blood tests, if needed, to evaluate clotting time and possible risk for infection.
- Psychological evaluation to assess the patient’s ability to follow the treatment guidelines and protocols, as active patient participation is needed for spinal cord stimulation to work effectively
- Cardiac or medical clearance to determine suitability for the trial, use of anesthesia, or possible future implantation of the stimulator
If the above results are satisfactory, the patient may elect to have a spinal cord stimulator trial.
Step 3: Trial
For the spinal cord stimulation trial procedure, the treatment wires and stimulator are temporarily placed in the back or neck to determine if the treatment is effective in reducing pain.
See Recovery After Spinal Cord Stimulation Trial
Step 4: Spinal cord stimulator implantation
If the trial meaningfully reduces the patient’s pain, the next step is a minimally invasive surgical procedure to implant the wires and spinal cord stimulator under the skin.
What Is a Spinal Cord Stimulator?
An implanted spinal cord stimulator delivers electric current to the nerves in the spinal cord.
A nerve stimulator is a small battery-powered generator designed to deliver mild electrical pulses to the nerves surrounding the spinal cord. It is about the size of a matchbox and can remain implanted under the patient’s skin for years, similar to a cardiac pacemaker.
Common areas for stimulator implantation are:
- Above the buttock or by the side of the abdomen2 – for treating back pain
- In the chest area – for treating neck pain
Before implanting the device, the treatment is tried for about 1 week to check if the electric stimulation is effective in treating the patient’s pain. During the trial, the stimulator is worn in a belt outside the patient’s body. If the trial is successful, the patient may decide to proceed with surgical implantation of the device.
An implanted stimulator does not cause pain or discomfort to the patient. Some people feel a small bump where the stimulator is implanted, but it is less likely to be visible when covered by clothing.
How a Spinal Cord Stimulator Works
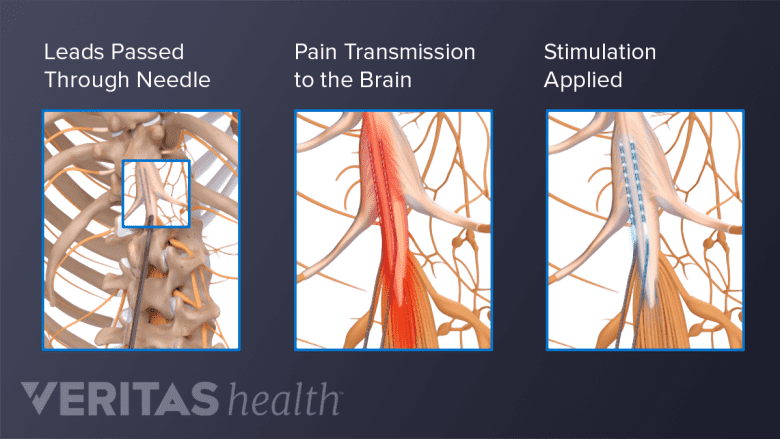
The leads are placed near specific nerves in the spine and inhibit pain signals passing through those nerves.
A spinal cord stimulator is designed to reduce chronic pain through the following mechanisms:
- The battery-powered stimulator device that connects to the electrodes is placed under the skin.
- The stimulator is connected to thin wires called leads, which have 10 to 30 electrodes (areas that give out the electric current).
- The electrodes are positioned near the pain-transmitting nerves in the spinal epidural space – a space surrounding the spinal cord that contains a network of nerves – in the neck or low back.
- When the stimulator generates electric current, the impulses reach the target nerves and alter the pain signals that pass through them – preventing the signals from reaching the brain.
The patient controls the spinal cord stimulator with a wireless remote control. The remote control is used to turn the device on or off and adjust the settings, such as the timing and frequency of the electric impulses.
Goals of Spinal Cord Stimulation Treatment
Spinal cord stimulation for neck or low back pain aims to accomplish one or more of the following goals:
- Reduce pain by at least 50%3
- Increase walking speed and distance (walking tolerance)3
- Increase the ability to perform daily activities of living and/or work3
- Improve the quality and quantity of sleep3
- Decrease reliance on pain medications, such as opioids or other potentially sedating medications, minimizing the potential for side effects and complications associated with long-term drug use
Through these goals, electric nerve stimulation helps patients manage their pain, but it does not eliminate the source of pain.
When Spinal Cord Stimulation Is Recommended
A trial with a spinal cord stimulator is considered for individuals with moderate to severe chronic pain who haven't found relief from nonsurgical or surgical treatments.
- Before surgery: A combination of non-surgical treatments is tried for at least 1 year before considering spinal cord stimulation. In some cases, spinal cord stimulation is recommended after a 6-month course of unsuccessful nonsurgical treatments, or for patients who are not surgical candidates.4 ,5
- After surgery: Spinal cord stimulation is most commonly recommended for people who have unresolved pain or develop new pain and symptoms despite spinal surgery and further surgery is not recommended.
Types of Electric Stimulation
There are broad categories of electric frequency and strength used in spinal cord stimulation:
Low-frequency stimulation
Also called tonic stimulation, this system delivers low-frequency electric current at 60 to 100 Hz. It produces a tingling sensation (paresthesia) in the area(s) where the patient previously experienced pain, such as the low back, leg, neck, or arm. Many individuals get used to the tingling feeling, while others find it uncomfortable.2
High-frequency stimulation
This system uses higher frequencies of 10 to 50 kHz. Patients do not feel anything when the stimulator is turned on. High-frequency stimulation produces better pain relief than low-frequency stimulation.2
Burst stimulation
In burst stimulation, constant low-frequency stimulation is used at 40 Hz, and a high-frequency burst of five pulses is delivered at regular intervals (every few seconds). Each burst has a frequency of 500 Hz, which produces minimal or no tingling.2
Success Rates of Spinal Cord Stimulation
A successful spinal cord stimulation treatment is defined as at least a 50% improvement in both pain and the ability to function and perform daily activities.3
Spinal cord stimulator trial success rates
Around 50% to 90% of people who undergo a spinal cord stimulation trial have successful outcomes.6
Individuals with a successful trial are eligible for permanent stimulator implantation. However, a successful trial does not guarantee long-term pain relief after the implantation.
Implanted spinal cord stimulator success rates
Around 50% to 80% of people have successful outcomes after a permanent spinal cord stimulator implant.7
Success rates of implanted spinal cord stimulation over time:
| Success rates of high-frequency stimulators | Success rates of low-frequency stimulators |
|---|---|
| Back pain and leg pain | |
| ~85% reduction in back and leg pain after 3 months | ~50% reduction in back and leg pain after 3 months |
| ~75% reduction in back and leg pain after 1 year | ~50% reduction in back and leg pain after 1 year |
| ~65% reduction in back and leg pain after 2 years | 40% to 45% reduction in back and leg pain after 2 years |
| Neck pain and arm pain | |
| 75% to 90% reduction in neck pain and arm pain for up to 1 year | Low-frequency stimulators are not well-researched for treating neck pain and arm pain. |
Factors affecting success rates
The amount of pain relief achieved through spinal cord stimulation depends on many factors, including but not limited to:
- The skill and experience of the physician performing the procedure
- The patient’s underlying condition
- The severity and duration of the symptoms
- The type of electric stimulation used
- Adherence to post-trial and/or post-implant care and rehabilitation
- The patient’s overall health and lifestyle factors, such as smoking or nicotine intake and fitness level
More research is needed to further establish the safety, efficacy, and long-term success of spinal cord stimulation in managing chronic pain conditions.
Types of Spinal Cord Stimulators
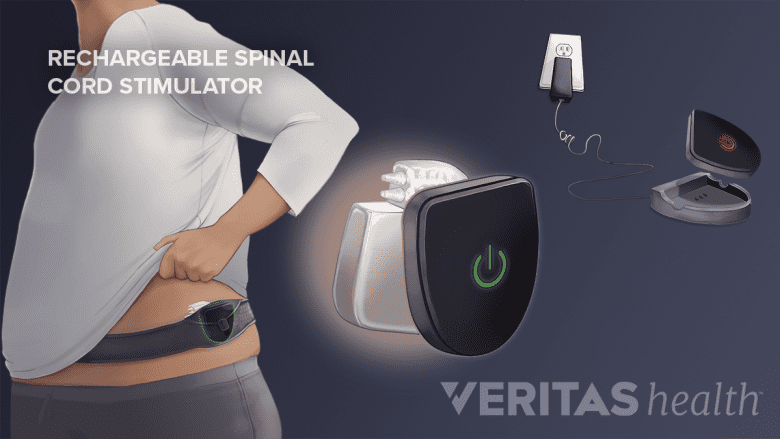
Rechargeable devices in the lower back are charged by wearing a belt around the waist.
Nerve stimulators are available in two types: rechargeable and non-rechargeable.
- Rechargeable stimulators have batteries that can be charged by the patient. They last for about 8 to 10 years, or more, after which, they need to be surgically replaced. They are charged by wearing a charger belt around the waist or chest (depending on the location of the stimulator) for about an hour.
- Non-rechargeable stimulators are slightly bigger but simpler to use because they do not need to be charged. However, they require a surgical replacement every 2 to 5 years to change the battery. This type of stimulator is beneficial for patients who are unable to or do not wish to charge their stimulator.
Some devices are constantly active and others are switched off and on, as needed, with the remote control.
Spinal Cord Stimulators and MRI Scans
Some stimulators are compatible with magnetic resonance imaging (MRI) scanners, but certain restrictions apply, such as the type of MRI machine, the magnet and scanner inside the machine, and the patient’s position.8 The patient must be awake and alert state to provide feedback if pain or discomfort is felt during the scan.
Depending on the type of stimulator device, it may be switched to MRI mode, programmed to the lowest setting, or turned off.
For people who anticipate needing MRI scans, having an MRI-compatible implanted stimulator may be an advantage.
For those with older models of the implanted spinal cord stimulator, it is likely that the device is not approved for MRI scans, increasing the risk of excessive heating of the stimulator wire (lead) and potential nerve damage if an MRI scan is performed.
Spinal Cord Stimulation Advantages
Potential advantages of spinal cord stimulation include:
- Treatment may be stopped at any time. If a person decides to discontinue the therapy at any time, the implanted wires and stimulator can be removed and there are no permanent changes to the spine.
- Adjustable pain relief. The number of pain adjustment options on the hand-held stimulator controller continues to grow as new models are introduced. It is usually a welcome change for individuals with chronic pain to have some control over pain management.
- Minimally invasive procedures. The trial process and permanent implant surgery are relatively small, minimally invasive procedures, causing minimal tissue disruption or blood loss.
- Reduced opioid use. For many people, spinal cord stimulation offers adequate pain relief, eliminating or reducing the need for pain-relieving medication. Up to 40% of patients either reduce their opioid usage or stop taking opioids after spinal cord stimulation treatment.9
- Targeted pain relief. Spinal cord stimulation delivers pain relief only where it is needed, reducing the risk of medication-related side effects, such as sedation, addiction, or constipation.
- Cost-effective pain relief. Research has determined the cost associated with spinal cord stimulation compares favorably with alternative treatments, including non-surgical therapies.10
- Alternative to oral medication. Spinal cord stimulation therapy offers a pain control option for those who have problems taking oral medication.
- No refills are needed. Pain relief from spinal cord stimulation is designed to last for years, without a need for new pills or frequent office visits.
- Facilitates rehabilitation. Pain relief afforded by a spinal cord stimulator allows many to engage in physical therapy and other types of rehabilitation, providing a better healing environment for the underlying spinal condition and reducing the likelihood of new or worsening conditions.
Spinal cord stimulation does not typically eliminate all pain but has the potential to significantly reduce the pain. Achieving this level of pain control and cutting back on—or eliminating—reliance on prescription pain-relieving medication makes the therapy helpful for many.
Read about Disadvantages and Risks of Spinal Cord Stimulation
Specialists Who Perform Spinal Cord Stimulator Implant
Specialists trained in interventional pain management are qualified to implant spinal cord stimulators. These specialists include anesthesiologists, physiatrists, orthopedic spine surgeons, and neurosurgeons.

