Spinal cord stimulation (SCS) is increasingly being used for hard-to-treat chronic pain. This treatment typically involves implanting a small device underneath the skin in the lower back or neck. The SCS device then sends mild electrical signals to the spinal cord near the pain source via wires and electrodes. It is believed that spinal cord stimulation can interfere with and reduce the pain signals before they travel up the spinal cord to the brain.
Most SCS devices contain a battery that must eventually be surgically replaced. With rechargeable SCS, the battery can theoretically last several years longer than with traditional SCS.
In This Article:
- Rechargeable Spinal Cord Stimulators for Chronic Pain
- When to Consider Getting a Rechargeable SCS
- Recharging a Rechargeable SCS
- Risks of Rechargeable SCS
Pain Conditions Commonly Managed By SCS
Some pain conditions that are more likely to respond favorably to SCS treatment include:
Failed back surgery syndrome. When surgery has failed to relieve back or neck pain, the result is typically called failed back surgery syndrome and may even result in the pain worsening. This condition is the most common reason for SCS treatment to be sought.
See Failed Back Surgery Syndrome (FBSS): What It Is and How to Avoid Pain after Surgery
- Complex regional pain syndrome (CRPS). CPRS typically involves an intense or burning pain that mysteriously spreads to an entire limb, such as the leg or arm. CRPS can occur with nerve damage from an injury, or it may result from a defect in the central nervous system that does not show up on imaging.
- Arachnoiditis. This condition involves the painful inflammation of the spinal cord’s outer layer.
SCS may also be considered for other causes of chronic pain, such as heart problems and various conditions that cause nerve damage.
When to Avoid Rechargeable SCS
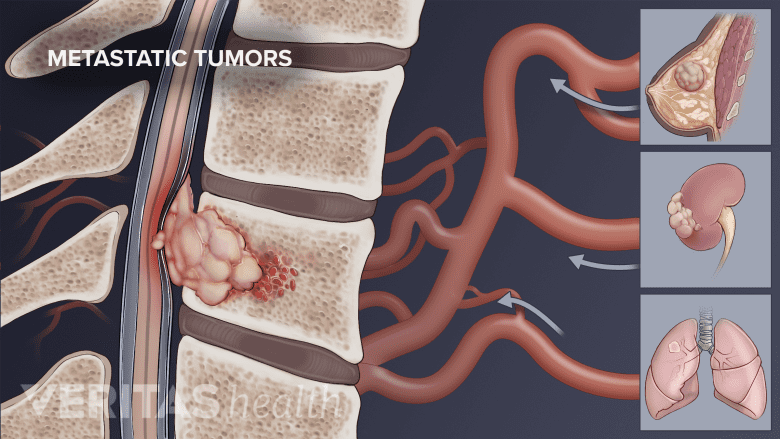
Spinal cord stimulation (SCS) is not recommended for patients with cancer.
If a patient anticipates that it would be inconvenient or uncomfortable to regularly recharge the SCS device, which may take many hours per week and increase as time goes on, opting for a standard (non-rechargeable) SCS device instead could make more sense. Although, it should be noted that many rechargeable devices can be charged in less than 1 hour per day, which can be done while watching TV or having a meal.
In addition, SCS should be avoided if:
- The pain is unlikely to be alleviated by stimulation, such as pain from cancer
- A medical condition would make the procedure unsafe, such as already having a pacemaker
- Untreated mental health issues are present, such as anxiety or depression
This is not a complete list of reasons to avoid getting SCS. For example, if spine surgery has a good chance of correcting the problem causing pain, it is typically recommended instead of implanting an SCS device.
See Spinal Cord Stimulator Implantation Surgery: Step by Step
Effectiveness of Rechargeable SCS
The exact mechanism by which spinal cord stimulation works to reduce pain is still unknown.1 However, the medical literature increasingly indicates that SCS can be an effective treatment for appropriately-selected candidates dealing with chronic pain in the spine and/or limbs.2 Some research indicates that spinal cord stimulation is more effective at reducing pain felt in a limb, such as the leg, rather than in the spine, such as the lower back,2 ,3 but there can still be meaningful back or neck pain relief.
It should also be noted that the effectiveness of SCS treatment can greatly depend on the doctor’s skill, product type, and other factors.
See Disadvantages and Risks of Spinal Cord Stimulation
While rechargeable SCS in theory should be more cost effective than traditional SCS in the long run due to fewer replacement surgeries needed, this is not always the case. For example, if rechargeable SCS has complications that require a procedure to either remove or replace the device, the potential cost-effectiveness is negated.
Also, if an insurance company is covering the procedure, the upfront costs to the patient tend to be the same regardless of whether a non-rechargeable or rechargeable device is implanted.
Editor’s Top Picks
- Spinal Cord Stimulation for Chronic Back Pain Video
- Who May Benefit from Spinal Cord Stimulation
- Spinal Cord Stimulation for Chronic Neck Pain Video
- Failed Back Surgery Syndrome (FBSS): What It Is and How to Avoid Pain after Surgery
- Spinal Cord Stimulation for Chronic Back and Neck Pain
- Recovery After Spinal Cord Stimulator Implant Surgery

