A standard first-line treatment approach for piriformis syndrome includes a focus on carefully and progressively stretching the piriformis muscle through guided physical therapy.1Probst D, Stout A, Hunt D. Piriformis Syndrome: A Narrative Review of the Anatomy, Diagnosis, and Treatment. PM & R, 11 Suppl 1. https://doi.org/10.1002/PMRJ.12189 Physical therapy and exercise for piriformis syndrome aim to reduce buttock pain; improve muscle function in the lower back, buttock, and thigh; and prevent a recurrence of symptoms.
Research indicates that most people experience complete symptom relief within 1-3 weeks after starting an exercise program for piriformis syndrome.2Hicks BL, Lam JC, Varacallo M. Piriformis Syndrome. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448172/
In This Article:
- Physical Therapy and Exercise for Piriformis Syndrome
- Stretching Exercises for Piriformis Syndrome
- Strengthening Exercises for Piriformis Syndrome
- Aerobic Exercises for Piriformis Syndrome
When Physical Therapy Is Recommended for Piriformis Syndrome
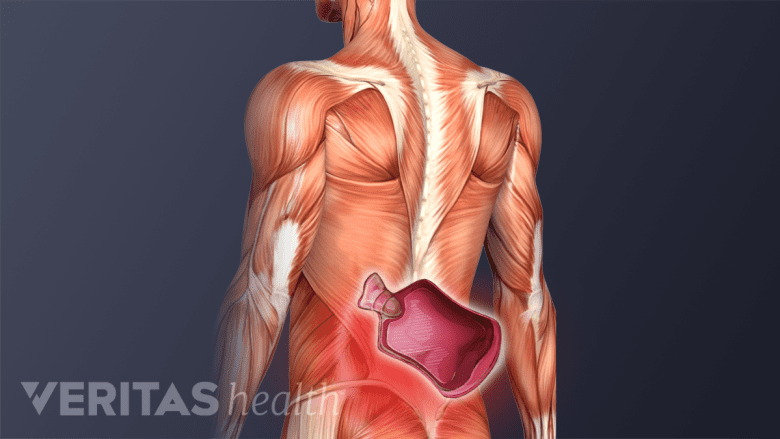
Physical therapy is advised for both acute and chronic cases of piriformis syndrome.
Physical therapy may be recommended for both acute and chronic piriformis syndrome. The treatment may be initiated as early as possible once the diagnosis is confirmed and serious medical conditions are ruled out.
Personalized treatment plans usually include a combination of exercises, passive techniques, and physical therapy aids to help treat and prevent the recurrence of piriformis syndrome symptoms.
Physical Therapy for Piriformis Syndrome: What to Expect
Physical therapists use modalities such as heat therapy to loosen tissues before an exercise program.
As one of the first-line treatments, physical therapy aims to provide long-term improvement and symptom control through a set of 5 treatment aspects described below.
- Educating the patient
Physical therapists provide guidance on proper body mechanics, posture, and lifestyle modifications that may help reduce or prevent the recurrence of symptomatic piriformis syndrome.
- Controlling pain and inflammation
Physical therapists use techniques such as massage, ultrasound, and heat or ice therapy to help reduce inflammation, pain, and discomfort.
- Improving flexibility
Once the inflammation and pain are under control, the physical therapist focuses on improving flexibility through guided techniques and flexibility exercises to perform at home.
A few guided flexibility techniques include:
- Stretching the piriformis through reciprocal inhibition
Reciprocal inhibition occurs when the contraction of one muscle leads to the relaxation of its opposing muscle.3Gulledge BM, Marcellin-Little DJ, Levine D, Tillman L, Harrysson OLA, Osborne JA, Baxter B. Comparison of two stretching methods and optimization of stretching protocol for the piriformis muscle. Med Eng Phys. 2014.36(2):212-218 http://doi.org/10.1016/j.medengphy.2013.10.016 This type of muscle relaxation is a normal reflex that helps optimize muscle function and prevent injuries. In the treatment of piriformis syndrome, reciprocal inhibition can help relax the piriformis muscle and reduce muscle spasm and pain in the buttock—thereby improving hip and thigh range of motion.
Reciprocal inhibition of the piriformis muscle is caused by contracting the hip flexors, which helps relax the piriformis muscle.3Gulledge BM, Marcellin-Little DJ, Levine D, Tillman L, Harrysson OLA, Osborne JA, Baxter B. Comparison of two stretching methods and optimization of stretching protocol for the piriformis muscle. Med Eng Phys. 2014.36(2):212-218 http://doi.org/10.1016/j.medengphy.2013.10.016
Watch 4 Easy Stretches For Piriformis Syndrome Pain Relief Video
- Stretching the piriformis by post-isometric relaxation
Post-isometric relaxation (PIR) is a technique that involves contracting a muscle for a specific period of time, followed by a passive stretch of that muscle. The idea behind PIR is that the muscle may relax more after the contraction, creating a greater range of motion during the stretch. Post-isometric relaxation is beneficial for the piriformis muscle because it is a small muscle located deep in the buttock, which can otherwise be hard to stretch effectively.4Wright P. A comparison of post-isometric relaxation (PIR) and reciprocal inhibition (RI) muscle energy techniques applied to piriformis. International Journal of Osteopathic Medicine. 2008.11(4):P158-159. http://doi.org/10.1016/j.ijosm.2008.08.015
Performing PIR on the piriformis muscle involves contracting the muscle by squeezing it as tightly as possible for 6-10 seconds, followed by a passive stretch of the muscle with an exercise like the seated piriformis stretch while the muscle is in a relaxed state.
- Releasing the piriformis muscle through neuromuscular massage
Neuromuscular massage therapy, also called myofascial trigger point therapy or myofascial release, is a specialized form of massage therapy used to relieve pain and tension in the muscles and connective tissue (fascia) of the body. It involves applying sustained pressure to specific points in the muscle or fascia, known as “trigger points,” to release tension and improve mobility.5Kukadia HA, Malshikare A, Palekar TJ. Effect of Passive Stretching v/s Myofascial Release in Improving Piriformis Flexibility in Females – A Comparative Study. Indian Journal of Physiotherapy and Occupational Therapy. 2019.13(4):57. http://doi.org/10.5958/0973-5674.2019.00132.1
How to release the piriformis muscle through neuromuscular massage: Piriformis muscle release can be performed using a foam roller or a tennis ball to apply sustained pressure to focal areas of painful muscle spasm in the buttock. Another way to perform neuromuscular massage therapy on the piriformis muscle is through therapist-assisted stretching, where a trained physical therapist uses hands-on techniques to apply pressure on the muscle to release tension.6Ahmad Siraj S, Dadgal R. Physiotherapy for piriformis syndrome using sciatic nerve mobilization and piriformis release. Cureus. Published online December 26, 2022. doi:10.7759/cureus.32952
- Stretching the piriformis through reciprocal inhibition
- Increasing strength
Multiple studies have found that weakness in the hip abductor muscles is commonly associated with piriformis syndrome and can be a contributing cause of buttock pain.7Tonley JC, Yun SM, Kochevar RJ, Dye JA, Farrokhi S, Powers CM. Treatment of an Individual with Piriformis Syndrome Focusing on Hip Muscle Strengthening and Movement Reducation: A Case Report. Journal of Orthopaedic & Sports Physical Therapy. 2010.40(2):103-111. https://www.jospt.org/doi/10.2519/jospt.2010.3108,8Barton PM. Piriformis syndrome: a rational approach to management. Pain. 1991.47:345-352. https://pubmed.ncbi.nlm.nih.gov/1784505/,9Hallin RP. Sciatic pain and the piriformis muscle. Postgrad Med. 1983.74:69-72. https://pubmed.ncbi.nlm.nih.gov/6878094/ Strength training exercises focused on targeting the muscles surrounding the piriformis, including the hip abductor and extensor muscles, may improve the recovery time as opposed to only targeting the piriformis muscle.6Ahmad Siraj S, Dadgal R. Physiotherapy for piriformis syndrome using sciatic nerve mobilization and piriformis release. Cureus. Published online December 26, 2022. doi:10.7759/cureus.32952 When the muscle strength in these muscle groups increases, it improves the overall hip and leg function.
- Developing endurance
The final step of a physical therapy program is to develop endurance in the muscle groups to help maintain muscle balance even when the region is fatigued.
Engaging in aerobic exercises, such as walking, low-impact cardiovascular exercise, or swimming, are common ways to develop muscle endurance and increase stamina. The potential benefits of aerobic exercise include10Daenen L, Varkey E, Kellman M, Nijs J. Exercise, Not to Exercise, or How to Exercise in Patients With Chronic Pain? Applying Science to Practice. Clin J Pain. 2015.31(2):108-114 http://doi.org/10.1097/AJP.0000000000000099:
- Reducing pain. Cardiovascular exercises can help to reduce pain and discomfort caused by piriformis syndrome by increasing blood flow to the affected area and promoting the release of endorphins, which are natural pain-relieving chemicals in the body.
- Improving muscle function. Cardiovascular exercises help improve muscle function by increasing the oxygen supply to muscles, which helps reduce muscle tension and improve the range of motion.
A regular routine of cardiovascular exercise also helps improve cardiovascular and lung health.
Duration of a Physical Therapy Program for Piriformis Syndrome Pain
The guidelines for treating piriformis syndrome are usually similar to treating most other musculoskeletal problems. The total length of an exercise program depends on the severity and duration of the symptoms and signs.
Physical therapy typically starts with a few sessions performed under the guidance of a therapist followed by a longer-term home program. If the pain and other symptoms resolve, no further visits are needed, and the home exercises may be continued.
For maximum benefit and pain relief, it is essential to comply with the exercise program as guided by the physical therapist. A vast majority of people experience a recurrence of symptoms if they do not continue their home exercise program once they have completed physical therapy.2Hicks BL, Lam JC, Varacallo M. Piriformis Syndrome. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448172/
Should Exercise be Avoided with Piriformis Syndrome: What You Need to Know
There are no specific exercises to avoid with piriformis syndrome, but some patients may find that certain exercises worsen their symptoms. If engaging in a specific exercise worsens the symptoms and causes significant discomfort with daily activities, the exercise may be temporarily avoided or modified. Continuing a regular exercise program is important; as long as it does not worsen the symptoms, it is safe and healthy to perform.11George SZ, Fritz JM, Silfies SP, et al. Interventions for the Management of Acute and Chronic Low Back Pain: Revision 2021. J Orthop Sports Phys Ther. 2021.51(11):CPG1-CPG60. http://doi.org/10.2519/jospt.2021.0304
Modifying exercises to manage buttock pain
If buttock pain worsens while sitting or bending, upright exercises like walking may be a good alternative. If buttock pain worsens with walking or standing, low-impact exercises (such as cycling) or seated exercises may be opted.
Watch 2 Walking Tips for Piriformis Syndrome Video
A physical therapist is trained to provide the most appropriate exercises to help minimize the pain caused by piriformis syndrome.
Stretching and strengthening exercises of the piriformis muscle frequently cause soreness in the buttock area when starting a physical therapy program. Improving the flexibility, strength, and endurance of the piriformis muscle helps diminish ongoing soreness. Any activity that exacerbates piriformis syndrome should be discontinued. If the pain does not subside, consultation with a physical therapist or physician is necessary.
When Physical Therapy Is Not Recommended for Piriformis Syndrome
Physical therapy is not recommended when severe nerve compression, tumors, or other serious medical conditions are suspected. A comprehensive evaluation from a physician who specializes in musculoskeletal medicine is required in such cases.12Boyajian-O’Neill LA, McClain RL, Coleman MK, Thomas PP. Diagnosis and management of piriformis syndrome: an osteopathic approach. J Am Osteopath Assoc. 2008.108(11):657-664. http://doi.org/10.7556/jaoa.2008.108.11.657,13Vij, N. Kiernan H, Bisht R, et al. Surgical and Non-surgical Treatment Options for Piriformis Syndrome: A Literature Review. Anesth Pain Med. 2021.11(1):e112825. http://doi.org/10.5812/aapm.112825
- 1 Probst D, Stout A, Hunt D. Piriformis Syndrome: A Narrative Review of the Anatomy, Diagnosis, and Treatment. PM & R, 11 Suppl 1. https://doi.org/10.1002/PMRJ.12189
- 2 Hicks BL, Lam JC, Varacallo M. Piriformis Syndrome. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448172/
- 3 Gulledge BM, Marcellin-Little DJ, Levine D, Tillman L, Harrysson OLA, Osborne JA, Baxter B. Comparison of two stretching methods and optimization of stretching protocol for the piriformis muscle. Med Eng Phys. 2014.36(2):212-218 http://doi.org/10.1016/j.medengphy.2013.10.016
- 4 Wright P. A comparison of post-isometric relaxation (PIR) and reciprocal inhibition (RI) muscle energy techniques applied to piriformis. International Journal of Osteopathic Medicine. 2008.11(4):P158-159. http://doi.org/10.1016/j.ijosm.2008.08.015
- 5 Kukadia HA, Malshikare A, Palekar TJ. Effect of Passive Stretching v/s Myofascial Release in Improving Piriformis Flexibility in Females – A Comparative Study. Indian Journal of Physiotherapy and Occupational Therapy. 2019.13(4):57. http://doi.org/10.5958/0973-5674.2019.00132.1
- 6 Ahmad Siraj S, Dadgal R. Physiotherapy for piriformis syndrome using sciatic nerve mobilization and piriformis release. Cureus. Published online December 26, 2022. doi:10.7759/cureus.32952
- 7 Tonley JC, Yun SM, Kochevar RJ, Dye JA, Farrokhi S, Powers CM. Treatment of an Individual with Piriformis Syndrome Focusing on Hip Muscle Strengthening and Movement Reducation: A Case Report. Journal of Orthopaedic & Sports Physical Therapy. 2010.40(2):103-111. https://www.jospt.org/doi/10.2519/jospt.2010.3108
- 8 Barton PM. Piriformis syndrome: a rational approach to management. Pain. 1991.47:345-352. https://pubmed.ncbi.nlm.nih.gov/1784505/
- 9 Hallin RP. Sciatic pain and the piriformis muscle. Postgrad Med. 1983.74:69-72. https://pubmed.ncbi.nlm.nih.gov/6878094/
- 10 Daenen L, Varkey E, Kellman M, Nijs J. Exercise, Not to Exercise, or How to Exercise in Patients With Chronic Pain? Applying Science to Practice. Clin J Pain. 2015.31(2):108-114 http://doi.org/10.1097/AJP.0000000000000099
- 11 George SZ, Fritz JM, Silfies SP, et al. Interventions for the Management of Acute and Chronic Low Back Pain: Revision 2021. J Orthop Sports Phys Ther. 2021.51(11):CPG1-CPG60. http://doi.org/10.2519/jospt.2021.0304
- 12 Boyajian-O’Neill LA, McClain RL, Coleman MK, Thomas PP. Diagnosis and management of piriformis syndrome: an osteopathic approach. J Am Osteopath Assoc. 2008.108(11):657-664. http://doi.org/10.7556/jaoa.2008.108.11.657
- 13 Vij, N. Kiernan H, Bisht R, et al. Surgical and Non-surgical Treatment Options for Piriformis Syndrome: A Literature Review. Anesth Pain Med. 2021.11(1):e112825. http://doi.org/10.5812/aapm.112825

