Surgery for cervical radiculopathy from a herniated disc should only be considered in those cases when 6 to 12 weeks of nonsurgical treatment fails to relieve neurological deficits in the arm, such as pain, numbness, and/or weakness.
In This Article:
- Cervical Radiculopathy from a Herniated Cervical Disc
- Cervical Radiculopathy from a Herniated Disc Treatment Options
- Surgical Options for Cervical Radiculopathy from a Herniated Cervical Disc
- Cervical Radiculopathy Interactive Video
An MRI scan or CT with myelogram can confirm the presence of a disc herniation and its specific location within the cervical spine. If the patient’s symptoms and neurological deficit match the results of the scan, surgery is very reliable in terms of relieving arm pain and has a low complication rate.1Rhee JM, Yoon T, Riew KD. Cervical radiculopathy. J Am Acad Orthop Surg. 2007; 15(8): 486-94.
See Cervical Herniated Disc Causes and Diagnosis
In general, neck surgery to relieve cervical radiculopathy symptoms from a herniated disc is done one of two ways: through the front of the neck (anterior approach) or through the back of the neck (posterior approach).
Anterior Approach to Treat Herniated Cervical Disc
When a herniated disc in the neck is treated surgically, it is usually with an anterior approach to remove the entire disc, called discectomy. Two common types of this surgery include:
- Anterior cervical discectomy with fusion (ACDF). This procedure involves the surgeon approaching the cervical spine from the front and removing the entire herniated disc. Then the normal disc height is maintained by inserting a spacer (plastic, metal, or bone) and fusing the adjacent vertebrae together.
- Artificial cervical disc replacement. Similar to ACDF, this procedure removes the entire herniated disc from the front. However, instead of fusing the spine, the disc is replaced with an artificial disc with the goal of preserving movement at that vertebral level.
Most herniated discs are safer to reach via the anterior approach. Another benefit is that the larger muscles at the back of the neck go undisturbed. However, the anterior approach could cause swallowing to be painful or uncomfortable for a couple of days or weeks while recovering.
See Artificial Disc Vs. Anterior Cervical Discectomy and Fusion
Posterior Cervical Decompression (Microdiscectomy)
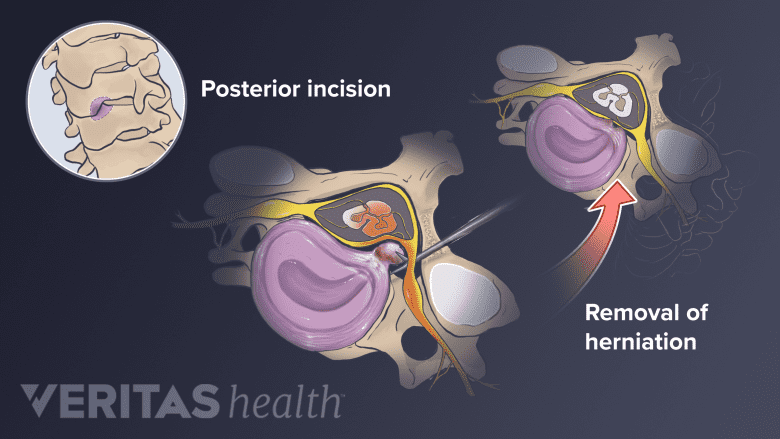
Posterior cervical decompression involves accessing the spine from the posterior (back) approach.
Sometimes surgeons remove part of a herniated disc while approaching the cervical spine from the back. This procedure, called posterior cervical decompression or microdiscectomy, tends to only be feasible if the herniated disc is located to the side of the spinal cord. A potential benefit of microdiscectomy is that no fusion is required, but a potential downside is that that the remaining disc material might herniate again.
Surgical Success Rate for Treating Cervical Radiculopathy

Surgery for cervical radiculopathy is usually successful and restores the quality of life for most individuals.
All surgeries have some risk, including the possibility of acquiring a life-threatening infection. However, surgery to treat cervical radiculopathy symptoms from a herniated disc is relatively safe and predictable.
See Potential Risks and Complications of ACDF Surgery
Regardless of whether the procedure is anterior or posterior, studies show that neck surgery to treat arm pain from cervical radiculopathy has an 80% to 90% success rate.1Rhee JM, Yoon T, Riew KD. Cervical radiculopathy. J Am Acad Orthop Surg. 2007; 15(8): 486-94. Patients can usually go home the next day and return to work within a week or two.
- 1 Rhee JM, Yoon T, Riew KD. Cervical radiculopathy. J Am Acad Orthop Surg. 2007; 15(8): 486-94.

