Physical therapy and exercise are typically first-line treatments for relieving, treating, and preventing sciatica symptoms. Typical sciatica signs and symptoms include:
- Lower back, hip, and/or leg pain
- Numbness, tingling, and/or weakness in the buttock, thigh, leg, and/or foot
Underlying medical conditions, such as a herniated or degenerated disc, or nerve root compression in the lumbar spine may cause radiating symptoms into the leg, commonly known as sciatica.
In This Article:
- Physical Therapy and Exercise for Sciatica
- Physical Therapy Aids and Passive Techniques for Treating Sciatica
- Video: 9 Exercises for Sciatica Pain Relief
- Sciatica Treatment Video
The Essentials of Physical Therapy for Sciatica
In treating sciatica, physical therapy may:
- Provide symptom relief
- Promote healing of the underlying cause
- Prevent recurrences and flareups
Several types of health professionals specialize in providing medical care and treatment for radiating lower back pain, including physical therapists, chiropractors, physiatrists (also called physical medicine and rehabilitation physicians), and certified athletic trainers. Physical therapists are specifically trained in providing manual therapy, exercise programs, and rehabilitation for radiating lower back pain.
8 Goals of Physical Therapy and Exercise in Treating Sciatica
Physical therapy for sciatica focuses on strengthening lower back and hip muscles.
Physical therapy and exercise help strengthen and mobilize tissues in the lower back, pelvis, abdomen, buttocks, and thighs.
The goals of physical therapy and exercise in treating the signs and symptoms of sciatica are to:
- Restore pain-free functional movement patterns
- Relieve lower back, buttock, thigh, and leg pain
- Reduce muscle spasm
- Restore the function of the lumbar spine and the sacroiliac joint
- Improve mobility of the lower body
- Foster a better healing environment in the lower back
- Promote neurologic adaptations to reduce the perception of pain
- Prevent future pain flareups and reduce fear associated with movement
Commitment and frequency are important attributes to a successful treatment outcome when using physical therapy and exercise for sciatica. Physical therapy may or may not be combined with the use of pain-relieving treatments, such as over-the-counter (OTC) or prescription medications or epidural steroid injections.
Physical Therapy and Exercise Techniques for Treating Sciatica
A physical therapist may prescribe a combination of various types of physical, manual, soft tissue mobilization, and/or exercise therapies in treating sciatica. Specific exercises depend on the underlying cause of sciatica,1Pourahmadi MR, Taghipour M, Ebrahimi Takamjani I, Sanjari MA, Mohseni-Bandpei MA, Keshtkar AA. Motor control exercise for symptomatic lumbar disc herniation: protocol for a systematic review and meta-analysis. BMJ Open. 2016;6(9):e012426. Published 2016 Sep 27. doi:10.1136/bmjopen-2016-012426,2Slater J, Kolber MJ, Schellhase KC, et al. The Influence of Exercise on Perceived Pain and Disability in Patients With Lumbar Spinal Stenosis: A Systematic Review of Randomized Controlled Trials. Am J Lifestyle Med. 2015;10(2):136–147. Published 2015 Feb 16. doi:10.1177/1559827615571510 as well as other factors, such as the patient’s level of pain, overall conditioning, and the physical therapist’s training and experience.
The list below highlights the common techniques:
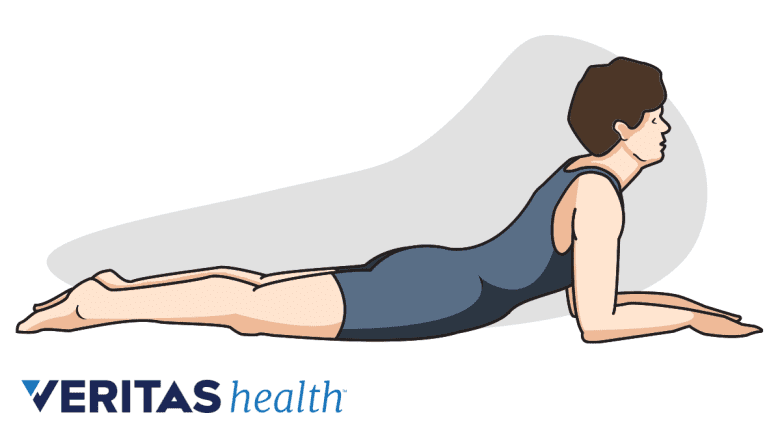
Extension and flexion back exercise
Flexion exercises are an essential component of physical therapy for sciatica.
These exercises help relieve pain by promoting spine movement. Often, individuals with lower back pain and sciatica feel relief with specific directional movement of the spine. A physical therapist typically evaluates an individual’s directional preference before prescribing specific directional exercises, as these are tailored to the individual patient and symptoms. These exercises include backward (extension) and forward (flexion) bending. This directional movement is an important component of the McKenzie Method, also known as mechanical diagnosis and therapy (MDT).
The McKenzie Method (mechanical diagnosis and therapy)
McKenzie's technique may reduce radiating symptoms by centralizing the pain closer to the spine.
The Mckenzie method is a technique that involves a series of active directional movements to identify and treat a pain source in the spine, muscles, and/or joints. The technique focuses on moving the radiating pain closer to the center of the body through exercise, for example, moving leg pain closer to the spine. The theory of this approach is that centralizing the pain indicates improvements in symptoms. The goal is to reduce radiating symptoms originating from the spine. A therapist who practices this technique usually has special training in the McKenzie Method.
Watch: Video: What Is the McKenzie Method?
Strengthening exercises
Leg raise is a type of core-strengthening exercise.
These exercises include bodyweight and resistance exercises to strengthen the muscles of the abdomen, low back, hips, and legs.
- Isometric exercises involve contracting muscles without moving the joints. Examples of isometric exercises include a plank or a bridge hold. These exercises can help strengthen muscles when symptoms are more acute.
- Isotonic exercises include the contraction of a muscle to resist a constant load, such as resistance bands and weight training, to help increase muscle strength through constant resistance to specific motions.
Read more about Back Strengthening Exercises
Functional retraining
This technique involves reintroducing movements, such as lifting, carrying, and bending or squatting. The use of proper technique and healthy movement patterns are incorporated to reduce pain and prevent re-injury.
Manual Therapy Techniques for Treating Sciatica
Specialized manual therapies for sciatica are discussed below.
Nerve glides (nerve mobilization)
Nerve glide includes active or passive techniques on a symptomatic nerve when it is placed into and out of tension to facilitate movement and reduce symptoms.
Joint mobilization and manipulation
Joint manipulation uses targeted force or pressure, aims to relieve pain, and improve joint mobility.
Joint manipulation and mobilization are manual techniques where a therapist applies quick, thrust force at the end range of the motion of a joint or pressure at joint to promote pain relief or restore joint movement.
Dry needling
Dry needling is a technique where a certified healthcare provider uses a small needle to target a trigger point in a muscle. This technique is performed to release hyper-irritable and/or hyper-contracted muscle tissue to reduce pain.
Muscle energy technique
This treatment is a form of manual therapy that involves the patient performing gentle muscle contractions in conjunction with the therapist moving the painful joints through a specific range of motion. This technique may help reduce pain and restore function.
Myofascial release and soft tissue mobilization
Manual soft tissue mobilization aims to reduce tension and spasms in tense muscle areas.
In this method, soft tissues are mobilized manually. The therapist uses their hands or an instrument to mobilize the tissues in the lower back, hips, or legs to treat fascial (underlying soft tissue) restrictions and decrease muscle tension or spasm.
See Myofascial Release Therapy
Gait training
A trained therapist analyzes the patient's walking technique and retrains the patient to use correct gait patterns. This technique may include video analysis.
Active assisted range of motion
This method involves therapist-assisted movement of parts of the lower body, such as the hip and legs. This technique helps facilitate the movement of specific joints or muscles that cause pain.
While this list is not exhaustive, therapists usually use one or more of these techniques in treating sciatica pain. If a particular exercise or therapy causes pain or discomfort, it is advised to inform the treating therapist immediately.
Read more about Physical Therapy for Low Back Pain Relief
Posture and Lifestyle Modifications for Sciatica
Using lumbar support while sitting helps support the spine.
In addition to physical therapy and exercise, committing to correct and ergonomically supported posture while sitting, standing, and walking is essential in treating and preventing sciatica. Daily routines, such as following ergonomically safe lifting techniques and using good sleep postures, are also important to follow.
Activity is more effective than bed rest
When sciatica is severe, patients may find the pain hard to bear and may need to rest a day or two. However, resting for more than a couple of days is generally not advised, as prolonged rest or inactivity can increase pain and lead to deconditioning. Regular movement is important to allow the flow of healing nutrients to the injured structures that cause pain.3Koes B. Moderate quality evidence that compared to advice to rest in bed, advice to remain active provides small improvements in pain and functional status in people with acute low back pain. Evidence-Based Medicine. 2010;15(6):171-172. doi:10.1136/ebm1132
While physical therapy is usually elective, meaning that it is the individual’s decision to participate or not, it is typically an essential component of resolving the signs and symptoms and aiding in the long-term prevention of sciatica.
- 1 Pourahmadi MR, Taghipour M, Ebrahimi Takamjani I, Sanjari MA, Mohseni-Bandpei MA, Keshtkar AA. Motor control exercise for symptomatic lumbar disc herniation: protocol for a systematic review and meta-analysis. BMJ Open. 2016;6(9):e012426. Published 2016 Sep 27. doi:10.1136/bmjopen-2016-012426
- 2 Slater J, Kolber MJ, Schellhase KC, et al. The Influence of Exercise on Perceived Pain and Disability in Patients With Lumbar Spinal Stenosis: A Systematic Review of Randomized Controlled Trials. Am J Lifestyle Med. 2015;10(2):136–147. Published 2015 Feb 16. doi:10.1177/1559827615571510
- 3 Koes B. Moderate quality evidence that compared to advice to rest in bed, advice to remain active provides small improvements in pain and functional status in people with acute low back pain. Evidence-Based Medicine. 2010;15(6):171-172. doi:10.1136/ebm1132