Most patients (over 75%) experience a full recovery with nonsurgical treatments, and adolescents have more favorable outcomes.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/,2Shamrock AG, Donnally III CJ, Varacallo M. Lumbar Spondylolysis and Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448122/
For individuals who are diagnosed with spondylolysis through imaging tests but do not experience any associated symptoms, no treatment is required, and no physical activity restrictions are needed.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
In This Article:
- Spondylolysis and Spondylolisthesis
- Symptoms and Diagnosis of Spondylolysis
- Spondylolysis Treatment
- Lumbar Spondylolysis Video
Self-care and Activity Restriction
For symptomatic spondylolysis, activity modification and other forms of self-care are recommended, and specifically include1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/,3Selhorst M, Allen M, McHugh R, MacDonald J. REHABILITATION CONSIDERATIONS FOR SPONDYLOLYSIS IN THE YOUTH ATHLETE. Int J Sports Phys Ther. 2020 Apr;15(2):287-300. PMID: 32269862; PMCID: PMC7134351.,4Goetzinger S, Courtney S, Yee K, Welz M, Kalani M, Neal M. Spondylolysis in Young Athletes: An Overview Emphasizing Nonoperative Management. J Sports Med (Hindawi Publ Corp). 2020 Jan 21;2020:9235958. doi: 10.1155/2020/9235958. PMID: 32047822; PMCID: PMC7001669.:
- Taking rest when the pain flares
- Stopping any activity, movement, or sport that increases the pain – typically activities that involve twisting or bending movements and or jarring the spine
- Using ice therapy to manage pain and reduce inflammation
- Applying a heating pad to the affected area to facilitate healing
- Using the log-rolling technique while getting in and out of bed. Log rolling involves rolling the body as one unit, keeping shoulders and hips in line – which helps avoid twisting or bending movements of the spine
- Supporting the natural inward curve of the low back by:
- Inserting a lumbar roll between the lower back and the chairback while sitting
- Placing a pillow under the knees while lying down to reduce stress on the lower back
- Placing a pillow between the knees when lying on the side to keep the spine in alignment
Implementing these tips helps preserve the spine's neutrality, reduce stress on the affected vertebra, facilitate healing, and reduce pain.
Medications to Relieve Spondylolysis Pain
Non-steroidal anti-inflammatory drugs (NSAIDs) help reduce pain and inflammation associated with spondylolysis.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/ Common examples include ibuprofen, naproxen, and aspirin. If NSAIDs cannot be taken, acetaminophen helps reduce pain.
These drugs are available over the counter and via a prescription (if higher strength is necessary).
It is important to note that some NSAIDs may not be suitable for all patients due to the potential risk of gastric irritation and cardiac problems. To avoid these risks, consulting a physician before taking these medications is advisable.
See Potential Risks and Complications of NSAIDs
Physical Therapy and Exercise

Strengthening exercises help restore and strengthen the functionality of the muscles of the lower back.
A guided course of physical therapy that emphasizes core exercise strengthening and stretching exercises is an essential component of spondylolysis treatment.2Shamrock AG, Donnally III CJ, Varacallo M. Lumbar Spondylolysis and Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448122/,3Selhorst M, Allen M, McHugh R, MacDonald J. REHABILITATION CONSIDERATIONS FOR SPONDYLOLYSIS IN THE YOUTH ATHLETE. Int J Sports Phys Ther. 2020 Apr;15(2):287-300. PMID: 32269862; PMCID: PMC7134351.
Physical therapy for spondylolysis focuses on1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/,3Selhorst M, Allen M, McHugh R, MacDonald J. REHABILITATION CONSIDERATIONS FOR SPONDYLOLYSIS IN THE YOUTH ATHLETE. Int J Sports Phys Ther. 2020 Apr;15(2):287-300. PMID: 32269862; PMCID: PMC7134351.:
- Motor control exercises: exercises that aim to restore the functionality of muscles that power and support the spine
- Lower back stabilization exercise: an exercise technique that relies on proprioception, or the awareness of where one’s joints are positioned, to help stabilize the muscles that support the spine
- Strengthening exercises: exercises that focus on strengthening and restoring functionality in specific muscle groups such as the deep abdominal and lumbar multifidus muscles
- Stretching exercises: exercises that focus on stretching the hip flexors, hamstrings, and quadriceps
- Progressive resistance training: which includes gradually introducing strength and resistance training, as tolerated by the patient
The duration of physical therapy varies on the individual’s specific condition and the severity and extent of spondylolysis, but on average, at least 6 weeks of therapy is usually recommended.2Shamrock AG, Donnally III CJ, Varacallo M. Lumbar Spondylolysis and Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448122/
Lumbar Bracing
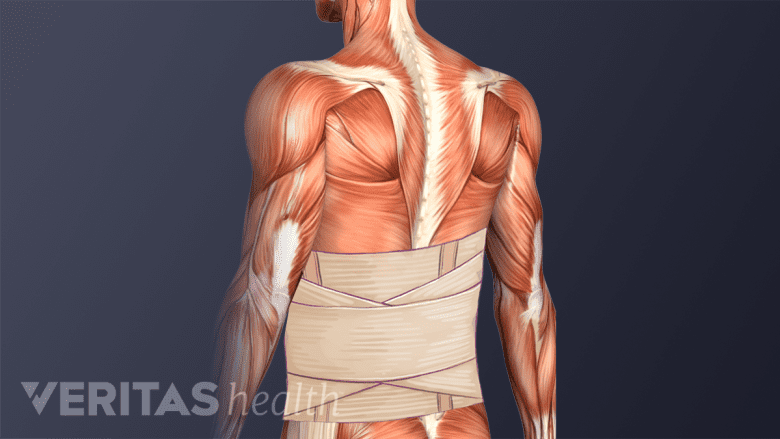
A lumbar brace can help stabilize the spine and assist in the recovery process.
Limited evidence suggests that using a lumbar (low back) brace for 6 to 12 weeks helps restrict motion in the low back, reducing stress on the weak pars interarticularis bone and promoting spondylolysis healing.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
However, several large-group studies that evaluated the effects of bracing did not find conclusive results to prove the long-term benefits of this treatment. Bracing may be used when other nonsurgical treatments fail to provide symptom relief.3Selhorst M, Allen M, McHugh R, MacDonald J. REHABILITATION CONSIDERATIONS FOR SPONDYLOLYSIS IN THE YOUTH ATHLETE. Int J Sports Phys Ther. 2020 Apr;15(2):287-300. PMID: 32269862; PMCID: PMC7134351.
Other Approaches to Treating Spondylolysis
If the above treatments do not work, if the symptoms are severe, and/or if progression to spondylolisthesis is suspected, the following treatments may be considered1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/:
- Lumbar epidural steroid injections
- Massage therapy
- Manual manipulation
- Cognitive-behavioral therapy (CBT)
Children and adolescents are almost always treated with some combination of nonsurgical treatments and surgery is rarely considered.4Goetzinger S, Courtney S, Yee K, Welz M, Kalani M, Neal M. Spondylolysis in Young Athletes: An Overview Emphasizing Nonoperative Management. J Sports Med (Hindawi Publ Corp). 2020 Jan 21;2020:9235958. doi: 10.1155/2020/9235958. PMID: 32047822; PMCID: PMC7001669.
Surgery for Spondylolysis
Surgical treatment for spondylolysis may be considered when1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/:
- Non-surgical treatments have been tried for at least 6 months or longer without satisfactory improvement in symptoms
- The neurological symptoms and signs of spondylolysis have progressed over time
- There is evidence of progression to a severe grade of spondylolisthesis (grade 3 or higher)
It is important to note that surgery may not always be completely effective, and some individuals may continue to experience lingering pain and restricted range of motion in the lumbar spine.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Types of Surgery for Spondylolysis
Laminectomy is a minimally invasive surgery used to treat spondylolysis.
Surgery aims to provide internal fixation and enhance the stability of the affected vertebra or spinal segment. Common procedures include:
- Laminectomy: a minimally invasive spinal decompression surgery that helps relieve compression of a spinal nerve root
- Lumbar spinal fusion surgery: a surgery designed to stop the motion at a painful vertebral segment in the low back.
- Direct repair of the defect in the pars interarticularis using screws (typically performed on vertebrae between L1 to L4).
It is essential to discuss the risks, benefits, and surgical alternatives with the surgeon before considering surgery for spondylolysis.
Patients are encouraged to work closely with their treating physician to develop a tailored treatment plan that addresses their specific needs and ensures the best possible outcome. Early diagnosis, prompt intervention, and ongoing care are vital in achieving successful results and optimizing the long-term well-being of individuals with spondylolysis.
- 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
- 2 Shamrock AG, Donnally III CJ, Varacallo M. Lumbar Spondylolysis and Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448122/
- 3 Selhorst M, Allen M, McHugh R, MacDonald J. REHABILITATION CONSIDERATIONS FOR SPONDYLOLYSIS IN THE YOUTH ATHLETE. Int J Sports Phys Ther. 2020 Apr;15(2):287-300. PMID: 32269862; PMCID: PMC7134351.
- 4 Goetzinger S, Courtney S, Yee K, Welz M, Kalani M, Neal M. Spondylolysis in Young Athletes: An Overview Emphasizing Nonoperative Management. J Sports Med (Hindawi Publ Corp). 2020 Jan 21;2020:9235958. doi: 10.1155/2020/9235958. PMID: 32047822; PMCID: PMC7001669.

