Some of the terms used when trying to diagnose neck or back pain can be confusing. Making matters even more complicated, medical professionals may use different terms to refer to the same condition.
Here are some commonly confused terms to know when discussing neck or back pain.
In This Article:
- Getting an Accurate Back Pain Diagnosis
- Commonly Confused Terms In Diagnosing Spinal Pain
Degenerative Disc Disease vs. Osteoarthritis

Facet joint osteoarthritis is a common degenerative condition of the spine.
Degenerative disc disease and osteoarthritis are two of the most common degenerative conditions of the spine.
- Degenerative disc disease is not actually a disease, but rather a degenerative process. As the intervertebral discs age, they naturally lose some hydration and height over time. Tears may develop in the disc’s protective outer layer, possibly leading to pain.
- Facet joint osteoarthritis occurs when the protective cartilage within one or more facet joints wears down between the vertebrae. The joint becomes swollen and arthritic as osteophytes (bone spurs) grow, enlarging the joint and causing more inflammation and potentially pain.
Degenerative disc disease and osteoarthritis typically occur simultaneously in the spine, because when either a disc or nearby facet joint starts to breakdown, it puts more pressure on the other. This process becomes recurrent and increases the likelihood of further degeneration of both these structures. Even when both of these conditions are present, medical professionals may refer to the problem differently depending on preferred terminology or which is causing the most problematic symptoms.
Read more: Facet Joint Disorders and Back Pain
Spondylosis is an umbrella term for spinal degeneration and its associated symptoms, which is also commonly used to describe facet joint osteoarthritis and/or degenerative disc disease.
Herniated Disc vs. Bulging Disc
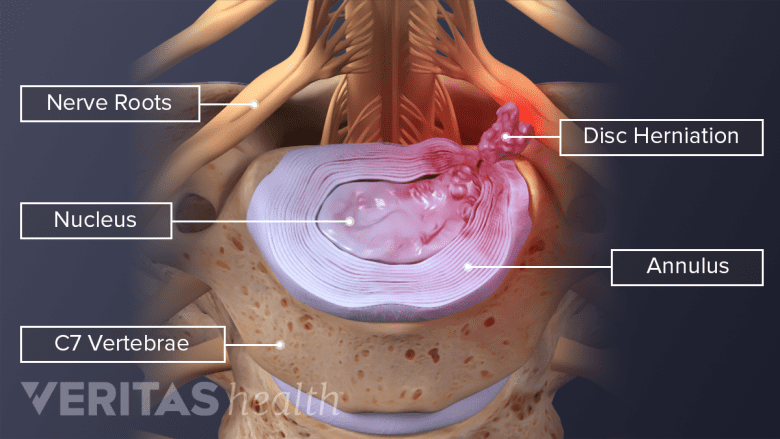
A herniated disc occurs when inflammatory proteins from a disc's inner core leak out.
A herniated disc is a common source of neck and back pain, but it is not always the same as a bulging disc.
- Bulging disc occurs when the disc’s protective outer layer (annulus fibrosus) bulges out beyond the vertebral body or normal disc space. In a bulging disc, the jelly-like inner portion (nucleus pulposus) does not leak into the outer layer.
- Herniated disc occurs when the disc’s nucleus pulposus starts to leak into cracks or tears in the outer layer. There are different stages of a herniated disc:
- Disc protrusion occurs when the nucleus pulposus leaks into the outer layer but not beyond its boundary.
- Disc extrusion occurs when the nucleus pulposus starts to leak beyond the boundary of the outer layer.
- Disc sequestration occurs when a part or fragment of the disc separates from the rest of the disc.
The terms ruptured disc or slipped disc may be used to refer to a herniated disc. It is important to note that even when a disc is herniated, it stays strongly attached to the adjacent vertebrae and does not actually slip.
Read more: What's a Herniated Disc, Pinched Nerve, Bulging Disc...?
Radiculopathy vs. Radicular Pain
Radicular pain occurs due to nerve root inflammation and radiates into the limb.
It is common to hear the terms radiculopathy and radicular pain used interchangeably by doctors and patients alike. However, there is technically a difference.
- Radicular pain occurs when a nerve root becomes inflamed and radiates pain from the spine, such as to an arm or leg. Radicular pain can range from mild to sharp or electric-like, but it does not involve neurological deficits.
- Radiculopathy occurs when nerve root inflammation or damage causes a change in neurological function, which can be measured and verified. For example, cervical radiculopathy may involve numbness and/or weakness that goes into the arm or hand. If a neurological deficit cannot be verified, such as with electrodiagnostic testing, radiculopathy cannot be diagnosed.
While radiculopathy typically includes radicular pain, it is not a requirement.
Symptoms vs. Signs
Many doctors simplify language for patients by referring just to symptoms when meaning both symptoms and signs.
- Symptoms refer to the evidence of illness or injury that a person experiences or feels, but cannot prove or demonstrate for a doctor. A few examples include pain, tingling, fatigue, or nausea.
- Signs refer to the evidence of illness or injury that can be verified with a test or observation. Some examples include weakness, fracture, fever, or vomiting.
A case of chronic neck or back pain may be particularly hard to diagnose if there are only symptoms present without verifiable signs to help further narrow down what might be wrong.
When to Ask for Clarification
If a doctor or other medical professional uses an unfamiliar term or says something confusing when explaining a diagnosis, it is important to ask for clarification. Fully understanding the diagnosis can help a patient make better decisions about the treatment options.

