There are several types of tests used to provide images of and/or analyze areas of pathology. These are generally referred to as "diagnostic studies." The findings of the test(s) are used to inform the underlying cause of the patient’s back or neck pain. Depending on the sensitivity of the test, the physician may be able to pinpoint the source and extent of the injury to further assist in the diagnosis and treatment planning.
The diagnostic evaluation of back and neck pain is a multifaceted and complex undertaking and typically includes 3 steps:
- Medical history. The first step to successfully understanding the probable cause of pain lies in the thoroughness of the medical history provided by the patient.
- Physical examination. The medical history is typically followed by a detailed physical examination performed by the physician.
- Diagnostic studies. Following the first two steps, the underlying cause of pain may either be confirmed or need confirmation through diagnostic studies.
In This Article:
- Introduction to Diagnostic Studies for Back and Neck Pain
- X-Ray of the Spine
- Computerized Tomography (CT) Scan
- Computerized Tomography (CT) Scan with Myelogram
- Electromyography (EMG)
- Somatosensory Evoked Potentials (SSEP)
When a Diagnostic Study May Be Recommended for Back or Neck Pain
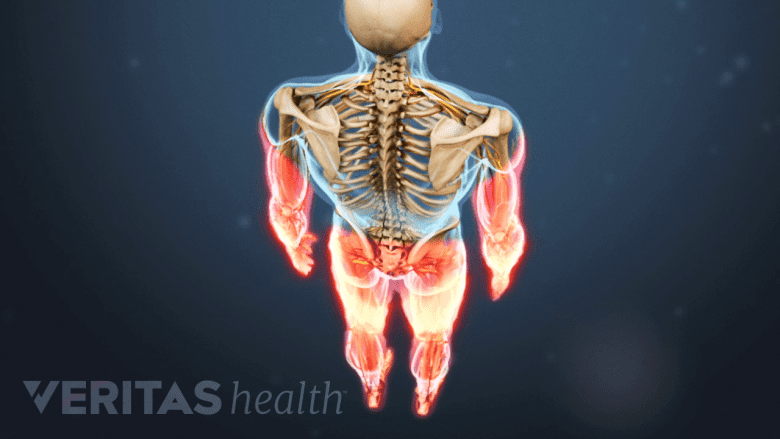
Diagnostic tests are recommended for red-flag symptoms like arm and/or leg weakness and numbness.
Findings from the medical history and physical exam typically set up the rationale for ordering diagnostic studies. Diagnostic tests are recommended when:
Red flag symptoms, including but not limited to fever, chills, night sweats, loss of bowel and/or bladder control, numbness in the arms and/or legs, loss of consciousness, not being able to stay alert, and/or feeling lightheaded and nauseous, are present
- A few underlying causes may be suspected but confirmation is needed to plan the appropriate treatment
- A potential cause is presumed but the exact location of the problem needs to be confirmed
- A systemic (general) disorder, such as infection or malignancy, is suspected
- Surgery is intended for the treatment of lower back or neck pain
Diagnostic tests may not be ordered when the cause of pain is established based on the judgment and experience of the physician, such as a general back muscle strain.
Types of Spinal Diagnostic Studies
The spinal tissues may be analyzed and studied through different mediums depending on the nature of the underlying problem. Commonly used studies are described below.
Imaging tests

MRI scans provide images for doctors to diagnose pain, plan treatment, and monitor progress.
Imaging, radiology, or radiographic tests, create standard or detailed images of certain areas inside the body, such as joints, bones, discs, organs, and soft tissues. The images obtained by these tests are used by doctors to analyze the tissues, in order to diagnose the underlying cause of pain, plan the treatment, or monitor the progress of treatment.
Examples of imaging tests include:
- X-rays
- Ultrasonography scans (or ultrasound scans)
- Computed tomography (CT) scans and CT scans with myelography (imaging using a contrast dye)
- Magnetic resonance imaging (MRI) scans
- Positron emission tomography (PET) scans
- Bone scans and bone scan with SPECT
Imaging tests are generally painless, relatively safe when used with standard precautions, and noninvasive. Selection of the appropriate imaging technique depends on the type of suspected pathology, general condition of the patient, availability, cost of the test, and the presence of certain contraindications, such as pregnancy.
Electrodiagnostic tests
Electrodiagnostic testing is used to analyze electrical activity in the muscles for the diagnosis of neuromuscular diseases. These tests help differentiate between myopathy (a disorder of the muscle) and neuropathy (a nerve disorder that causes muscle weakness and other symptoms) and monitor the response to treatment.1Chang CW. Electrodiagnostic medicine. In: Braddom’s Rehabilitation Care: A Clinical Handbook. Elsevier; 2018:44-48.e6.
Common electrodiagnostic tests for back or neck pain are electromyography (EMG) and nerve conduction studies (NCS). Less often, somatosensory evoked po¬tential (SSEP) testing can help provide additional information about spinal cord function. These tests record muscle and nerve activity to detect abnormalities that may not be physically obvious.
Blood tests
Blood tests may be used when the physician suspects inflammation, cancer, or inflammatory arthritis. Common blood tests recommended for these conditions may include:
Complete blood count (CBC): gives information about the production of all types of blood cells and identifies the oxygen-carrying capacity of the blood.
For back pain and neck pain, this test is helpful in diagnosing certain cancers and infections among other findings.
Erythrocyte sedimentation rate (sed rate): measures the viscosity of blood plasma by analyzing the tendency of red blood cells to aggregate and settle through the plasma, thereby marking the level of inflammation in the body.
For back pain and neck pain, this test may be used to detect inflammatory spinal arthritis, such as rheumatoid arthritis in the spine.
C-reactive protein (CRP): is an acute inflammatory protein that increases up to 1,000-fold with infection or inflammation.2Sproston NR, Ashworth JJ. Role of C-Reactive Protein at Sites of Inflammation and Infection. Front Immunol. 2018 Apr 13;9:754. doi: 10.3389/fimmu.2018.00754
For back pain and neck pain, this test may be used to detect rheumatoid arthritis and infection in the spine.
Research suggests that the C-reactive protein test is a better and more sensitive indicator of inflammation compared to the erythrocyte sedimentation rate (ESR). It also responds more quickly to changes in a clinical situation.3Harrison M. Erythrocyte sedimentation rate and C-reactive protein. Aust Prescr. 2015;38(3):93-94. doi:10.18773/austprescr.2015.034
Biopsy
A biopsy is the process of removal of cells or tissues for examination. For back pain and neck pain, a biopsy may be recommended when a tumor is suspected and may include4Tehranzadeh J, Tao C, Browning CA. Percutaneous needle biopsy of the spine. Acta Radiol. 2007;48(8):860-868. doi: https://doi.org/10.1080/02841850701459783:
- Percutaneous needle biopsy. In this biopsy, a needle is inserted through the skin and into the tumor using x-ray or ultrasound guidance. There are two types of percutaneous needle biopsy for the spine:
- Fine needle aspiration biopsy (FNAB): the process of obtaining a sample of cells and bits of tissue by applying suction through a fine needle attached to a syringe
- Core needle biopsy (CNB): procedure for extracting a cylindrical sample of tissue using a large, hollow needle
- Open biopsy. This biopsy is performed when surgery is already planned and may be incisional (removing a part of the tumor) or excisional (removing all of the tumor).
Percutaneous needle biopsy is a potentially safe and effective procedure and is commonly used when a confirmatory diagnosis is needed for lesions in the spine.4Tehranzadeh J, Tao C, Browning CA. Percutaneous needle biopsy of the spine. Acta Radiol. 2007;48(8):860-868. doi: https://doi.org/10.1080/02841850701459783
Factors That May Affect the Outcome of Diagnostic Test Results
The accuracy of specific diagnostic tests, such as blood tests or electrodiagnostic tests, can be altered due to illnesses, certain medications, stress, alcohol or caffeine consumption, and/or dehydration. It is important to discuss these factors with the doctor prior to scheduling an appointment. It is also possible to get false positive or false negative test results. If the samples are not adequate or suitable for testing, a re-test may be ordered.
For imaging tests, the quality of the test and the accuracy with which it is performed may affect the final image results. Obesity and excessive bowel gases may obscure important findings or make interpretation of the film difficult.5Hackett BA. The role of imaging in diagnosis of low back pain. Journal of Radiology Nursing. 2020;39(3):154-155.
Follow-up tests may be required if further investigation is needed and to make sure health problems are identified early, and that a patient is responding well to treatment.
Interpreting Diagnostic Test Results
A doctor who specializes in the field of the test reviews the result(s) and provides it to the treating physician, who eventually discusses it with the patient or caregiver.
Imaging tests, which are commonly used in back pain diagnoses, are read and interpreted by a radiologist. Blood samples and biopsy tissues are usually analyzed and interpreted by a pathologist. Documents with blood test results show a normal reference range for each type of finding that is listed, which makes it easy for patients to read and understand their test results.
In general, no single diagnostic study can provide all the answers, and most test results need to be interpreted in conjunction with other diagnostic information, such as the physical examination and medical history.
Read more about Getting an Accurate Back Pain Diagnosis
- 1 Chang CW. Electrodiagnostic medicine. In: Braddom’s Rehabilitation Care: A Clinical Handbook. Elsevier; 2018:44-48.e6.
- 2 Sproston NR, Ashworth JJ. Role of C-Reactive Protein at Sites of Inflammation and Infection. Front Immunol. 2018 Apr 13;9:754. doi: 10.3389/fimmu.2018.00754
- 3 Harrison M. Erythrocyte sedimentation rate and C-reactive protein. Aust Prescr. 2015;38(3):93-94. doi:10.18773/austprescr.2015.034
- 4 Tehranzadeh J, Tao C, Browning CA. Percutaneous needle biopsy of the spine. Acta Radiol. 2007;48(8):860-868. doi: https://doi.org/10.1080/02841850701459783
- 5 Hackett BA. The role of imaging in diagnosis of low back pain. Journal of Radiology Nursing. 2020;39(3):154-155.

