A cervical herniated disc can cause many different types of pain or no symptoms at all. The pain can range from an aching in the neck, arm, and/or hand to electric-like pain that radiates into these same areas. Sometimes arm or hand numbness or weakness may also be present. While a cervical herniated disc may originate from some sort of trauma or neck injury, the symptoms commonly start spontaneously.
Cervical herniated disc pain and related signs are typically felt in one arm or the other. Symptoms can vary depending on which disc has herniated and which nerve root has become pinched or inflamed. Rarely, the pain, tingling, numbness, and/or weakness can go into both arms or lower in the body if the spinal cord is affected. Loss of bowel and/or bladder control are also rare but possible outcomes.
In This Article:
- Cervical Herniated Disc Symptoms and Treatment Options
- Cervical Herniated Disc Signs and Symptoms
- Cervical Herniated Disc Causes and Diagnosis
- Conservative Treatment for a Cervical Herniated Disc
- Spine Surgery for a Cervical Herniated Disc
- Cervical Herniated Disc Video
Pain Management for a Cervical Herniated Disc
Ice and heat therapy are effective self-care treatments for herniated discs.
Neck and/or arm pain from a cervical herniated disc may be short-lived and only last for a few days, or it could become chronic and last for months or longer. It is common for the pain to come and go, or have particularly bad flare-ups during certain activities. When neck and/or arm pain stems from a herniated disc, the symptoms typically resolve completely within 4 to 6 months, even though the disc itself may not heal. 1 Wong JJ, Côté P, Quesnele JJ, Stern PJ, Mior SA. The course and prognostic factors of symptomatic cervical disc herniation with radiculopathy: a systematic review of the literature. Spine J. 2014; 14(8):1781-9.
Watch Video: Can Herniated Discs Heal on Their Own?
Most cases of cervical herniated disc pain can be successfully managed with nonsurgical treatments, such as over-the-counter pain medications, physical therapy to strengthen and stretch the neck, ice or heat packs, and/or activity modifications to avoid painful movements until the pain has subsided. Occasionally, oral steroids or an epidural or selective nerve root injection using x-ray guidance and contrast may be needed to help calm pain and advance rehabilitation.
How a Cervical Disc Herniates
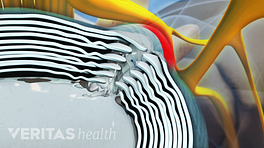
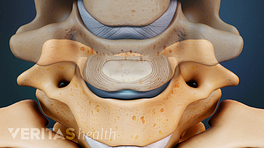
A herniated disc occurs when the inner core of the disc bulges through the outer covering.
There are 6 intervertebral discs in the cervical spine. Each cervical disc is situated between adjacent vertebrae (one above and one below) to cushion the vertebral bodies and help distribute loads from the neck and head above. A disc has 2 basic components.
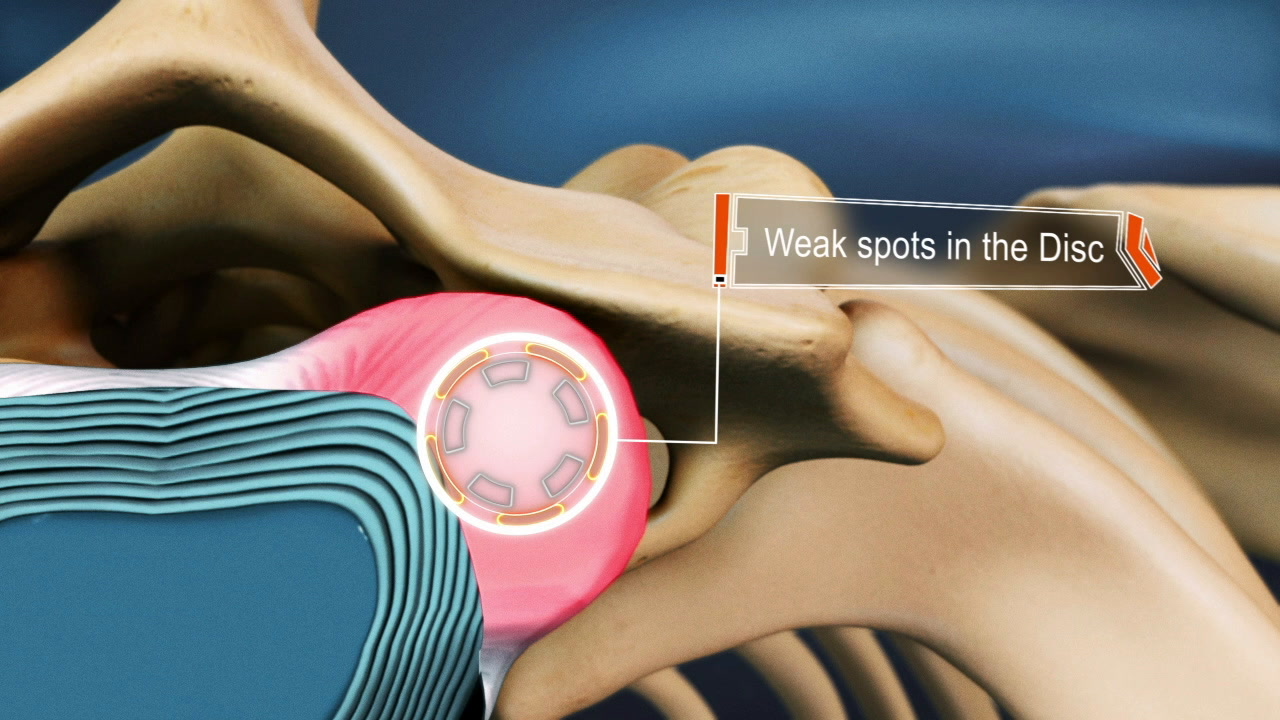
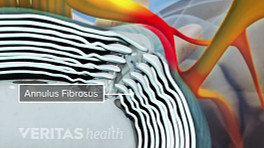
- Annulus fibrosus. This sturdy outer layer is constructed of concentric collagen fibers, which make the disc strong enough to shield its soft inner layer. The annulus fibrosus helps to handle the spine’s heavy loads and absorb shocks.
- Nucleus pulposus. This gel-like interior is a loose network of fibers suspended in mucoprotein gel and protected within the annulus fibrosus. The nucleus pulposus provides additional cushioning and flexibility for movements.
Read more about Cervical Discs
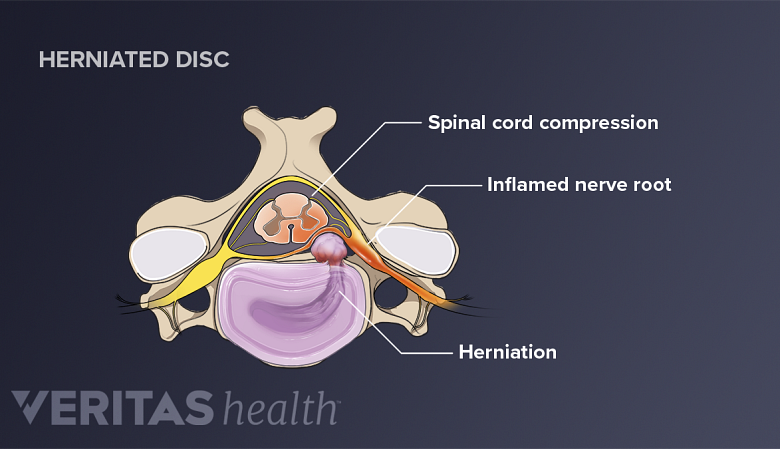
A herniated disc occurs when part or all of its protective outer layer tears and some of the nucleus pulposus leaks into the tear. A herniated disc typically causes the most pain when the nucleus pulposus, which contains inflammatory proteins, leaks out of the disc and onto a nearby nerve root. Less commonly, a herniated disc may leak onto the spinal cord.
Risk Factors for a Cervical Herniated Disc
The risk for developing a herniated disc tends to increase with age. Some estimates suggest that a cervical herniated disc is most likely to develop between ages 30 and 50. 2 Massa RN, Mesfin FB. Herniation, Disc. 2018 Oct 27. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441822/. PubMed PMID: 28722852. Most studies have found men to be at higher risk for a cervical herniated disc, 1 Wong JJ, Côté P, Quesnele JJ, Stern PJ, Mior SA. The course and prognostic factors of symptomatic cervical disc herniation with radiculopathy: a systematic review of the literature. Spine J. 2014; 14(8):1781-9. but a recent study suggests women may be at higher risk. 3 Kim Y-K, Kang D, Lee, Ilho, Kim S-Y. Differences in the incidence of symptomatic cervical and lumbar disc herniation according to age, sec and national health insurance eligibility: a pilot study on the disease’s association with work. Int J Environ Res Public Health. 2018; 15(10): 2094. doi: 10.3390/ijerph15102094.
The rate of cervical herniated discs occurring in the adult population has been estimated to be between 0.5% and 2%. 1 Wong JJ, Côté P, Quesnele JJ, Stern PJ, Mior SA. The course and prognostic factors of symptomatic cervical disc herniation with radiculopathy: a systematic review of the literature. Spine J. 2014; 14(8):1781-9. Although, many cases of cervical herniated disc may go undiagnosed and estimates could vary by population.
When a Cervical Herniated Disc Is Serious
Severe spinal nerve root compression may cause radiculopathy in the arm.
Rarely, a cervical herniated disc’s signs and symptoms may gradually feel worse rather than eventually stabilizing and resolving on its own. If a cervical nerve root remains pinched or inflamed, tingling, numbness, and/or weakness may progress in the arm. Similarly, if the spinal cord is compressed or inflamed by a cervical herniated disc, problems with walking, coordination, and/or reduced bladder or bowel control may be present. These types of neurological deficits require immediate medical attention to prevent them from worsening or becoming permanent.
- 1 Wong JJ, Côté P, Quesnele JJ, Stern PJ, Mior SA. The course and prognostic factors of symptomatic cervical disc herniation with radiculopathy: a systematic review of the literature. Spine J. 2014; 14(8):1781-9.
- 2 Massa RN, Mesfin FB. Herniation, Disc. 2018 Oct 27. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441822/. PubMed PMID: 28722852.
- 3 Kim Y-K, Kang D, Lee, Ilho, Kim S-Y. Differences in the incidence of symptomatic cervical and lumbar disc herniation according to age, sec and national health insurance eligibility: a pilot study on the disease’s association with work. Int J Environ Res Public Health. 2018; 15(10): 2094. doi: 10.3390/ijerph15102094.