Spondylolysis refers to a defect in the short, flat strip of bone called pars interarticularis (or pars). The pars is located at the back of the spine and forms a bridge (or isthmus) between the upper and lower joint surfaces of each facet of a vertebra (spinal bone).
Spondylolisthesis is a condition where a vertebra slips forward over the vertebra below it. When spondylolisthesis occurs due to spondylolysis, the condition is called isthmic spondylolisthesis.
Spondylolysis and isthmic spondylolisthesis rarely cause pain, but when symptoms do occur, they typically affect children and adolescents.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/,2Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560679/,3Mikhael MM, Shapiro GS, Wang JC. High-grade adult isthmic L5-s1 spondylolisthesis: a report of intraoperative slip progression treated with surgical reduction and posterior instrumented fusion. Global Spine J. 2012;2(2):119-124. doi:10.1055/s-0032-1307257 Spondylolysis occurs in the lumbar spine (low back) and primarily affects the L5 vertebra.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
In This Article:
- Spondylolysis and Spondylolisthesis
- Symptoms and Diagnosis of Spondylolysis
- Spondylolysis Treatment
- Lumbar Spondylolysis Video
Understanding Spondylolysis
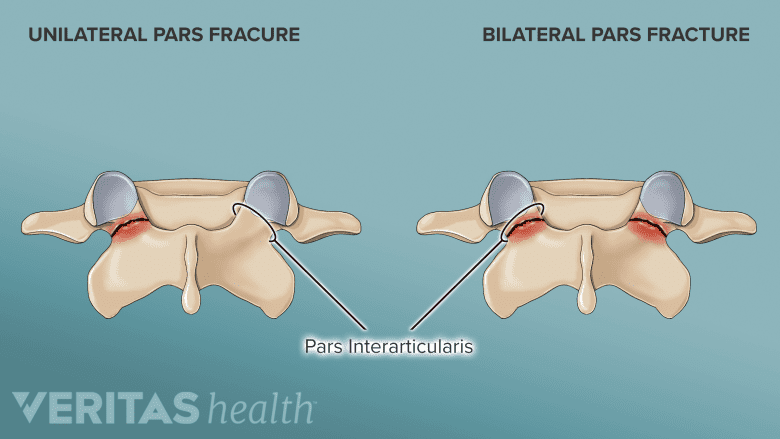
A stress fracture of the pars can occur on one side or both sides.
Spondylolysis occurs when a stress fracture in the pars does not fuse or heal completely as a part of the bone’s natural healing process, leaving the bone permanently split into two pieces.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Research shows that the pars is subjected to the greatest force compared to any other structure in the lumbar spine, making it vulnerable to stress fractures. In susceptible individuals, the pars may fracture, heal, and fracture again—repeatedly.4Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
The fracture can involve the right pars, left pars, or both. Pars fractures involving both sides (also called bilateral fractures) are more common than one-sided (or unilateral) fractures.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
A stress fracture of the pars can occur as a result of1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/,4Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/:
- Hereditary causes that make the pars more likely to fracture
- Weak bone tissue in the pars that is present at birth (congenital)
- Abnormally long pars bone
- Sudden trauma to the spine
The condition is more common in genetically susceptible children and adolescents who frequently participate in activities or sports that involve repeated forward bending and rotation of the spine. These actions, coupled with the genetic defect or weak bone tissue, cause excessive microtrauma to the growing, immature pars interarticularis, leading to a fracture.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Classic Symptoms and Signs of Spondylolysis
A dull ache in the lower back and buttock area is a common symptom of spondylolysis.
Spondylolysis pain feels like a dull ache that spans across the low back area. The buttocks and the back of the thigh may also feel sore, and the muscles in these areas tend to feel stiff or tight.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Bending backward or performing twisting movements increases spondylolysis pain in the low back.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
If there is associated isthmic spondylolisthesis, the symptoms may differ and include nerve pain, tingling, and leg weakness based on the severity of the vertebral slippage and spinal nerve compression.4Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
See Isthmic Spondylolisthesis Symptoms
Spondylolysis Causes and Risk Factors
Activities and sports that have a high impact on the spine may cause pars fractures.
In addition to those with high genetic susceptibility, the following individuals are also likely to be affected by spondylolysis1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/:
- Males (spondylolysis is twice as likely to occur in males than females)
- Children who are diagnosed with abnormal bone and nerve conditions such as spina bifida occulta, Marfan syndrome, or osteogenesis imperfecta
- Adolescents who are actively involved in high-impact sports
- Adults diagnosed with spinal osteopetrosis (weak, brittle bone)
Spondylolysis is usually identified during adolescence, around the age of 15, when symptoms start to manifest.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Specific sports that increase the likelihood of a pars fracture are1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/:
- Gymnastics and weightlifting
- Football, soccer, and rugby
- Basketball and volleyball
- Tennis
- Golf
- Swimming (butterfly and breaststroke)
Approximately 4% of 6-year-old children and 6% of teenagers aged 14 have this condition.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Progression of Spondylolysis to Isthmic Spondylolisthesis
When spondylolysis causes the vertebra to slip forward, it results in spondylolisthesis.
When a bilateral stress fracture of the pars interarticularis does not heal, the affected vertebra becomes incapable of bearing the heavy loads of the spine, causing the upper and lower surfaces of the facet joints to disconnect and separate. This separation makes the vertebra lose connection with the rest of the spine, resulting in isthmic spondylolisthesis – a forward slippage of the vertebral body, typically in a horizontal pattern.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Spondylolysis typically impacts the L5 vertebra in approximately 90% of cases, and if the condition progresses, L5 slips over S1.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
If only one of the pars interarticularis bone gets fractured (unilateral spondylolysis), the condition does not progress to isthmic spondylolisthesis.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
While spondylolysis is more common in adolescent males, the progression to isthmic spondylolisthesis is more common in adolescent females.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Spondylolisthesis can also occur due to degenerative changes in the spine (degenerative spondylolisthesis), trauma (traumatic spondylolisthesis), or bone diseases, such as spinal cancer (pathologic spondylolisthesis).
Why Spondylolysis Is More Common in Adolescents
The bone along the outer side of the upper joint surface of the facets has a small, rounded projection called the mammillary process. This bony projection serves as an attachment point for the thin strips of deep spinal multifidi muscles, which stabilize the facet joints and provide stability to the spine.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
The mammillary process is not completely formed until the age of 25, making the facet joint complex (which includes the pars) vulnerable to injury.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
A similar structure called the neural arch (an arch of bone at the back of a vertebra) also does not develop until the age of 25, contributing to the risk of spondylolysis and subsequent spondylolisthesis.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Progression to spondylolisthesis is less likely to occur in adults compared to adolescents.5Gagnet P, Kern K, Andrews K, Elgafy H, Ebraheim N. Spondylolysis and spondylolisthesis: A review of the literature. J Orthop. 2018 Mar 17;15(2):404-407. doi: 10.1016/j.jor.2018.03.008. PMID: 29881164; PMCID: PMC5990218.
The Course of Spondylolysis
Spondylolysis is not considered a serious condition and typically has an excellent long-term outlook when treated appropriately. For individuals with no symptoms, treatment, activity restriction, or other precautions are not needed.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
How long spondylolysis takes to heal
For symptomatic patients, complete healing generally occurs within 6 to 12 weeks of nonsurgical treatments. One-sided pars fractures heal sooner than bilateral fractures.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
In cases that have progressed to spondylolisthesis, the bone may not heal completely but the symptoms usually subside with treatment.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Return to work or play after spondylolysis
Over 75% of patients achieve complete relief from their symptoms with nonsurgical treatments.1, In adolescents, the healing process is more favorable, with approximately 92% of adolescent athletes returning to competitions after conservative treatment.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Surgery for spondylolysis is rare and when considered, about 90% of young athletes have a successful return to sports activities.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Potential complications of spondylolysis
While rare, if left untreated, spondylolysis may progress to spondylolisthesis and subsequent nerve or spinal cord damage if the vertebral slippage is severe.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Spondylolysis may also accelerate the progression of co-occurring degenerative spinal conditions, such as degenerative disc disease and spondylosis, potentially leading to severe spinal stenosis and lumbar radiculopathy.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
When to See a Doctor for Spondylolysis
Progressive weakness and numbness in the legs may require immediate medical attention.
Certain red flags suggest potential complications or severe underlying issues associated with spondylolysis and must be evaluated immediately by a medical professional. These signs and symptoms include but are not limited to:
- Progressive neurological symptoms. Progressive weakness, numbness, or tingling in the legs, or feet may indicate severe nerve compression due to spondylolysis-related spinal instability.
- Unrelenting pain. Experiencing intense and unrelenting back pain, especially after a traumatic event or fall, indicates a more serious injury or fracture.
- Bowel or bladder dysfunction. Difficulty controlling bowel or bladder movements, or experiencing urinary or fecal incontinence, may indicate cauda equina syndrome, a rare but severe complication of spondylolysis that requires urgent medical attention.
- Sudden worsening of symptoms. If the existing symptoms suddenly intensify, it could indicate a significant progression of the condition or a related complication.
- Pain at rest or night pain. Pain that persists when resting or worsens at night might indicate a more severe underlying problem, such as a spinal tumor.
- Fever or signs of infection. Fever, chills, and signs of infection (redness, swelling, or a discharge) around the back area may suggest an infection in the spine, which requires urgent medical assessment and treatment.
Recognizing these red flag signs and symptoms is vital to ensure timely intervention and prevent potential complications associated with spondylolysis.
Medical Professionals Who Treat Spondylolysis
If spondylolysis is suspected, it is advisable to consult with a qualified healthcare professional for a thorough evaluation and personalized treatment plan. Physiatrists (PM&R specialists), sports management specialists, orthopedic surgeons, physical therapists, and chiropractors have specialized training in managing musculoskeletal disorders and can effectively treat spondylolysis and spondylolisthesis.
- 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
- 2 Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560679/
- 3 Mikhael MM, Shapiro GS, Wang JC. High-grade adult isthmic L5-s1 spondylolisthesis: a report of intraoperative slip progression treated with surgical reduction and posterior instrumented fusion. Global Spine J. 2012;2(2):119-124. doi:10.1055/s-0032-1307257
- 4 Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
- 5 Gagnet P, Kern K, Andrews K, Elgafy H, Ebraheim N. Spondylolysis and spondylolisthesis: A review of the literature. J Orthop. 2018 Mar 17;15(2):404-407. doi: 10.1016/j.jor.2018.03.008. PMID: 29881164; PMCID: PMC5990218.