Most people with spondylolysis do not experience any symptoms. If symptoms are present, they are generally less severe and do not cause significant discomfort. However, if spondylolysis progresses to isthmic spondylolisthesis, the type and severity of symptoms tend to escalate.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Around 10% of patients with spondylolysis develop back pain and 50% to 75% of these symptomatic individuals have accompanying spondylolisthesis.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
In This Article:
- Spondylolysis and Spondylolisthesis
- Symptoms and Diagnosis of Spondylolysis
- Spondylolysis Treatment
- Lumbar Spondylolysis Video
Common Symptoms of Spondylolysis
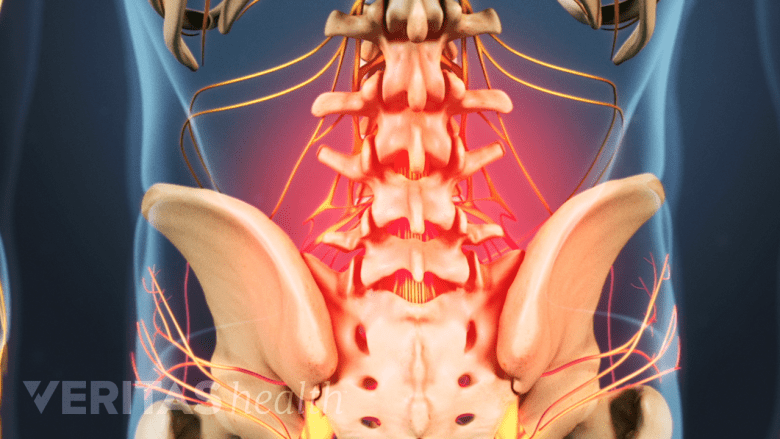
Lower back pain is a common symptom of spondylolysis.
The symptoms of spondylolysis develop over time and include1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/:
- Mild to severe back pain, which is typically described as a dull ache and may affect:
- The lower back area (axial back pain)
- The lower back, buttock, and back of the thigh
- Increase in pain while bending backward
The symptoms of spondylolysis come and go over time, with periods of relief followed by periods of symptom flare-ups.
Symptoms and Signs of Spondylolisthesis Caused by Spondylolysis
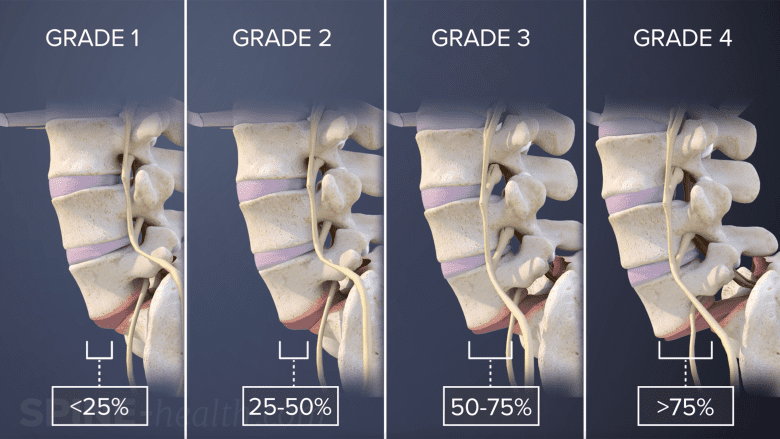
The severity of symptoms in isthmic spondylolisthesis depends on the grade of vertebral slippage.
The symptoms of isthmic spondylolisthesis vary depending on the severity of the condition and include some combination of2Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/,3Li N, Scofield J, Mangham P, Cooper J, Sherman W, Kaye A. Spondylolisthesis. Orthop Rev (Pavia). 2022;14(4):36917. Published 2022 Jul 27. doi:10.52965/001c.36917:
- Localized low back pain that may be described as a dull ache or sharp pain
- Back pain with sharp, shooting, or searing leg pain – also called sciatica – which occurs when the slipped vertebra presses on a nearby spinal nerve
- Muscle weakness, numbness, and/or abnormal sensation in various parts of the thigh, leg, or foot
- Pain in both legs while walking varying distances – also called neurogenic claudication
- An exaggerated curvature of the lower back causing lordosis (increased inward curving) or swayback
- A forward stooped posture
Activities that involve excessive backward bending or rotation of the torso usually exacerbate the symptoms, and the pain is relieved with rest.4Pereira Duarte M, Camino Willhuber GO. Pars Interarticularis Injury. [Updated 2023 Feb 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545191/
Read more about Isthmic Spondylolisthesis Symptoms
Diagnosis of Spondylolysis
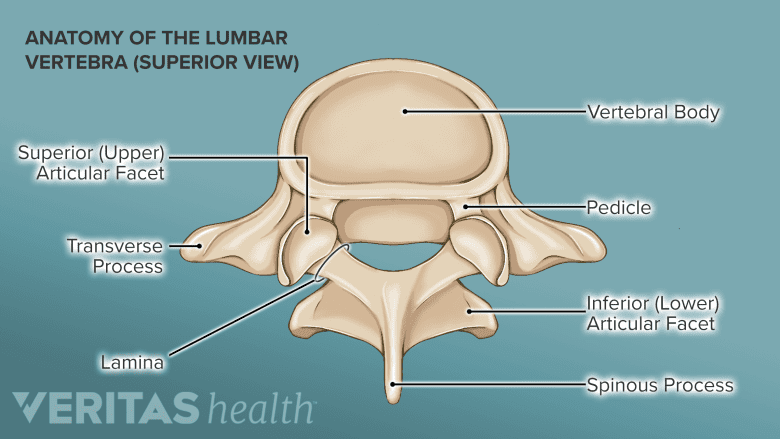
Analyzing the spinous processes of the lower back vertebrae helps identify spondylolisthesis.
A review of the patient’s symptoms and signs, clinical test(s), and imaging modalities are used to diagnose spondylolysis.
Review of symptoms and clinical tests for spondylolysis
In kids and teens, spondylolysis is usually the suspected cause of low back pain with or without leg pain.
Clinical tests used to identify spondylolysis and spondylolisthesis are:
- One-legged hyperextension maneuver: In this test, the patient stands on one leg and bends backward. If the test produces pain, it may indicate acute spondylolysis. The test is performed on both legs. This test is also called unilateral extension test or Michelis' test.
- Lumbar spinous process palpation: This test is done by a doctor and involves applying firm pressure to the bony protrusions (spinous processes) of the vertebrae while sliding the fingertips from the upper part of the lower back to the pelvis. If there is no lumbar spinous process or a noticeable "step," it may suggest the presence of spondylolysis that has advanced to spondylolisthesis.
If clinical tests are positive, the physician may order imaging tests to confirm the diagnosis.
Imaging tests to confirm the type of spondylolysis
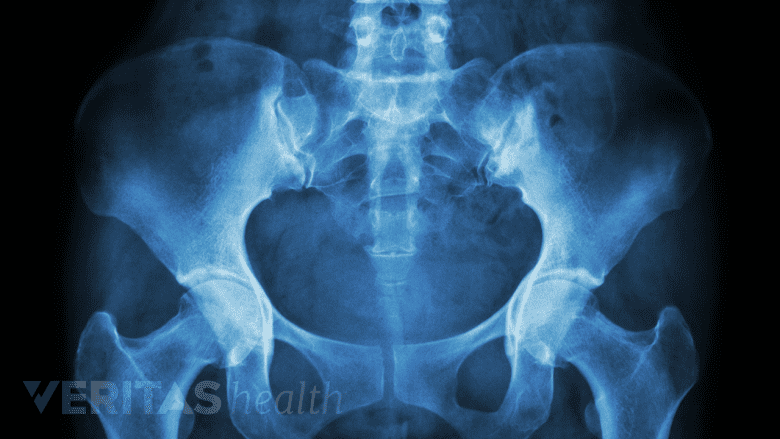
X-ray images may help in the diagnosis of spondylolysis.
An anterior (front), posterior (back), and lateral (side) x-ray is used to confirm the diagnosis. An oblique view x-ray helps determine if the spondylolysis is one-sided or has occurred on both sides.
To determine if the spondylolysis is active (causes acute symptoms) or inactive (has become chronic), a single-photon emission computed tomography (SPECT) bone scan or magnetic resonance imaging (MRI) scan may be ordered. These scans help evaluate the structural and functional changes that are associated with spondylolysis.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
- Active spondylolysis. On a SPECT scan, active spondylolysis shows uptake of the radiotracer agent, and an MRI scan shows bone marrow swelling adjacent to the pars defect. These findings indicate that there is activity or movement associated with the pars defect, which is likely to produce symptoms of low back pain.
- Inactive spondylolysis. If there are no indications of activity with the pars defect, then the spondylolysis is considered inactive and any low back pain experienced by the patient is probably incidental (meaning that there is another cause of the patient's lower back pain, such as a muscle strain).
Because spondylolysis is commonly found in children, there is a concern about exposing them to radiation. For this reason, if regular x-rays show no signs of the condition, the next preferred imaging method is usually an MRI, which can detect the changes associated with the pars fracture and provide detailed information on neural and soft tissue issues.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
The SPECT scan is useful in assessing the severity of a fracture. However, it involves radiation exposure, making it less desirable for use in pediatric cases, where minimizing radiation hazards is a priority.1McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
With early detection and appropriate interventions, individuals can experience relief from symptoms and achieve a favorable outcome.
- 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
- 2 Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
- 3 Li N, Scofield J, Mangham P, Cooper J, Sherman W, Kaye A. Spondylolisthesis. Orthop Rev (Pavia). 2022;14(4):36917. Published 2022 Jul 27. doi:10.52965/001c.36917
- 4 Pereira Duarte M, Camino Willhuber GO. Pars Interarticularis Injury. [Updated 2023 Feb 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545191/

