Surgery may be indicated for the treatment of severe isthmic spondylolisthesis when non-surgical treatments have failed to provide symptom relief.
Unless a medical emergency, spine surgery is typically elective, meaning that it is the patient's decision whether or not to undergo surgery. Patients are advised to discuss the risks, benefits, and alternatives to surgery with their physician before consenting to a surgical procedure.
In This Article:
- Isthmic Spondylolisthesis
- Isthmic Spondylolisthesis Symptoms
- Understanding the Causes and Diagnosis of Isthmic Spondylolisthesis
- Nonsurgical Treatment for Isthmic Spondylolisthesis
- Spinal Fusion Surgery for Isthmic Spondylolisthesis
- Isthmic Spondylolisthesis Video
When Surgery May be Recommended for Isthmic Spondylolisthesis
Severe pain that affects both legs may indicate a medical emergency.
Specifically, surgery is recommended when the following 3 criteria are present 1 Mohile NV, Kuczmarski AS, Lee D, Warburton C, Rakoczy K, Butler AJ. Spondylolysis and isthmic spondylolisthesis: a guide to diagnosis and management. J Am Board Fam Med. 2022;35(6):1204-1216. doi:10.3122/jabfm.2022.220130R1 , 2 Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560679/ :
- A combination of non-surgical treatments has been tried for at least 6 months
- There’s progressive worsening of symptoms
- Neurological symptoms, such as neurogenic claudication (leg pain while walking) and/or sciatica is present
In appropriately selected patients, surgical treatments have shown >80% success rates with a low rate of post-surgical risks and complications. 2 Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560679/
Types of Surgeries for Isthmic Spondylolisthesis
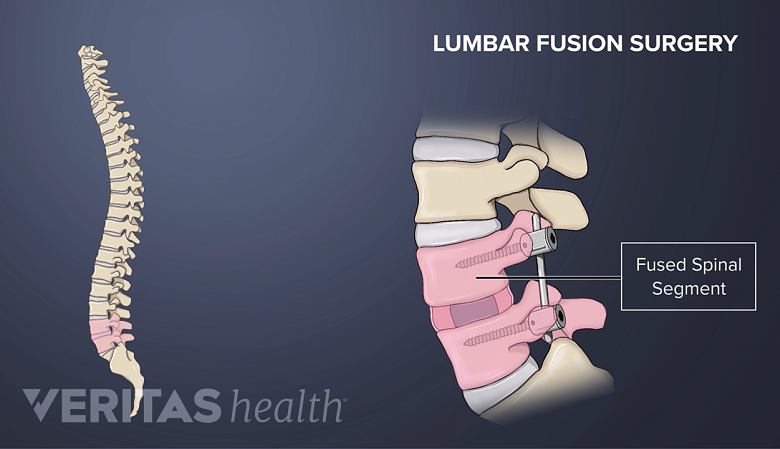
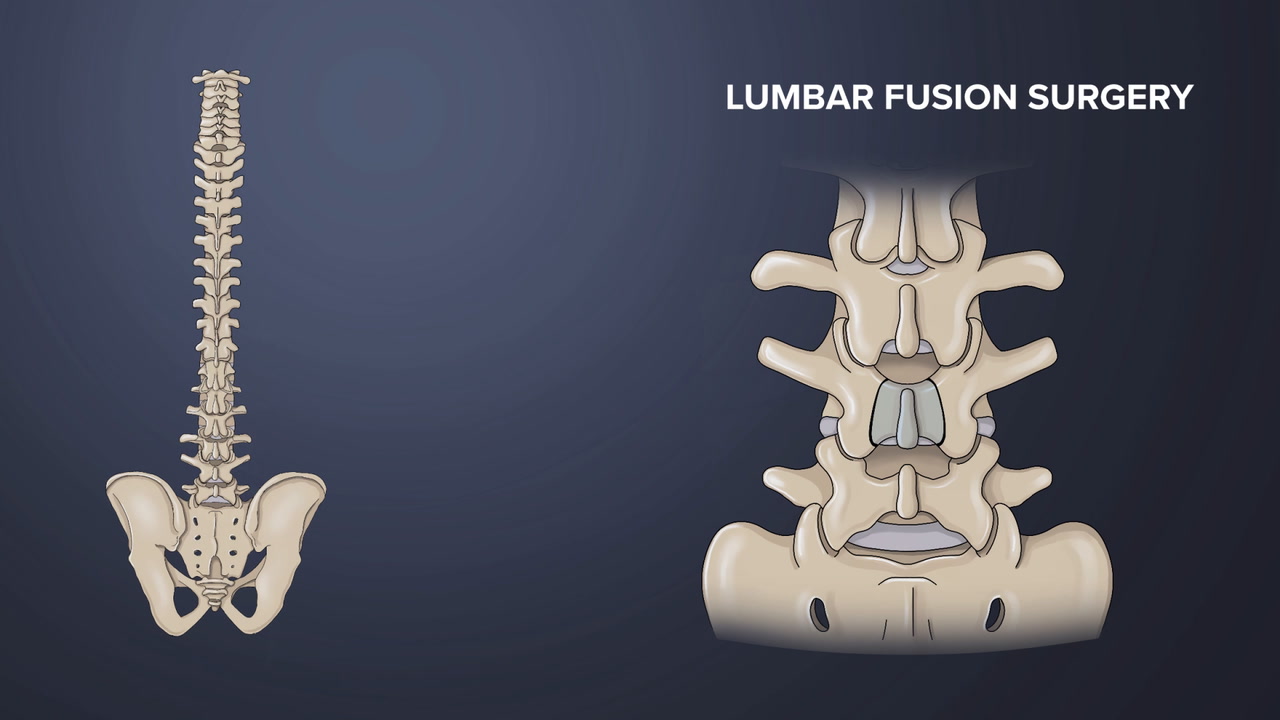
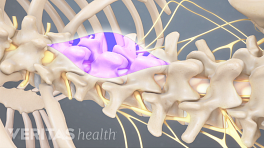
A spinal fusion surgery involves removal of the disc and fusion of adjacent vertebral segments.
Based on the grade and severity of isthmic spondylolisthesis, different types of surgeries may be used to treat the condition 2 Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560679/ :
- Posterolateral fusion (approached from the back) with pedicle screw instrumentation performed with lumbar decompression is generally considered the standard spinal surgery for isthmic spondylolisthesis. Watch Posterolateral Gutter Fusion Surgery Video
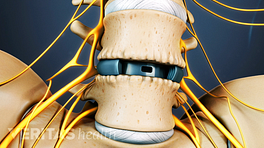
- Interbody fusion surgery including the anterior, posterior, transforaminal, and direct lateral interbody fusions (ALIF, PLIF, TLIF, and XLIF) with the insertion of a spinal cage may be performed in select patients.
- Removal of the L5 vertebra (vertebrectomy) and fusion of the L4 vertebra with the sacrum (S1) may be considered in severe L5 slips.
- Decompression without fusion may be indicated in some mild cases of grade 1 and 2 slips.
In children with pars interarticularis fracture or non-union of the pars, surgery with lag screw, tension band wire technique, or pedicle screw hook fixation may be considered. 2 Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560679/
An Individualized Approach is Essential
When surgically treating spondylolisthesis, it is essential to adopt an individualized approach that considers factors such as the severity of the condition, the predominant neurological symptoms, and any existing medical conditions. By doing so, surgeons can determine the most suitable treatment plan for each case.
Additionally, with the advancements in minimally invasive surgical techniques, patients with spondylolisthesis can receive tailored treatment plans that offer the best chance for successful outcomes and with quicker recovery and improved quality of life.
Bone Healing and Recovery After Fusion Surgery for Isthmic Spondylolisthesis
Understanding the recovery process after a spinal fusion surgery can help set realistic expectations and ensure a successful outcome.
Timeline for returning to daily activities
Most people are able to return home from the hospital about 2 to 4 days after lumbar spinal fusion surgery. Driving may be resumed a couple weeks after returning home and once the opioid medications have been stopped. It typically takes about 4 to 6 weeks to return to an office or sedentary job, but it can take 3 months or longer to return to activities that are more physical.
The exact duration of the recovery period varies for each individual. It is important to remember that everyone heals at their own pace, and patience is key during the recovery process.
See Postoperative Care for Spinal Fusion Surgery
Gradual rehabilitation: Gentle exercises and proper body mechanics for healing spine
Low-intensity aerobic exercises can help regain strength in the lower back
Physical therapists work with the patient to begin gentle exercises and teach proper body mechanics to protect the healing spine. A therapist creates a personalized rehabilitation program to gradually strengthen the back muscles, improve flexibility, and restore mobility. These exercises may initially focus on gentle movements and gradually progress to more challenging activities as the healing progresses.
See Physical Therapy for Low Back Pain Relief
Managing pain and discomfort after surgery
During the initial weeks and months, some pain and discomfort may be experienced, which is normal after surgery. The surgeon may recommend pain management techniques, such as prescribed medications or cold packs, to alleviate any discomfort. It is essential to communicate any concerns or unexpected symptoms to the surgeon without delay.
While fusion surgery can provide long-term stability and pain relief, it is crucial to follow the surgeon's instructions regarding post-surgical care, rehabilitation, and any recommended follow-up appointments for complete recovery with minimal complications.
- 1 Mohile NV, Kuczmarski AS, Lee D, Warburton C, Rakoczy K, Butler AJ. Spondylolysis and isthmic spondylolisthesis: a guide to diagnosis and management. J Am Board Fam Med. 2022;35(6):1204-1216. doi:10.3122/jabfm.2022.220130R1
- 2 Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560679/