While the neck’s naturally aging and degenerating spine typically causes no significant symptoms during a lifetime, that is not always the case. For people who do experience pain from cervical spine degeneration, symptoms may become severe, such as shock-like pain that radiates from the neck down the arm or pins-and-needles tingling/numbness/weakness that prevents normal use of the hand. Other people experience a constant dull aching pain, a grinding sensation when they move their neck, and progressive restriction of their range of motion.
One of the biggest mysteries associated with spinal degeneration is why it causes pain for some people but not others.
In This Article:
- How the Cervical Spine Changes With Age
- How Cervical Disc Degeneration Occurs
- How Cervical Facet Joint Degeneration Occurs
- How Neck Bones and Soft Tissues React to Spinal Degeneration
- When Does the Neck’s Spinal Degeneration Become Painful?
MRI Findings Can Be Misleading
Many people by their 30s have signs of degeneration in the cervical spine that would be visible on MRI imaging—and by age 70 almost everyone has it. 1 Teraguchi M, Yoshimura N, Hashizume H, et al. Prevalence and distribution of intervertebral disc degeneration over the entire spine in a population-based cohort: the Wakayama Spine Study. Osteoarthr Cartil. 2014; 22(1):104-10 However, an MRI alone is not a good indicator of whether a person is experiencing pain—or even where pain might be originating.
There have been cases where MRIs show severe spinal degeneration but the patients do not report any pain. The opposite has also been true—people report severe pain and yet only mild degeneration appears on MRI imaging.
Pain Mechanisms Still Being Studied
There are numerous conditions that can be caused by spinal degeneration. For most of these conditions, there are multiple ways they can manifest and cause pain—if they cause pain at all. Furthermore, multiple conditions can be present at once, and it may be hard to distinguish whether any or all of these conditions are contributing to symptoms.
See Neck Pain Causes
For example, a patient with neck pain could be diagnosed with cervical degenerative disc disease, cervical osteoarthritis, foraminal stenosis, spinal stenosis, and a herniated disc, but the exact cause(s) of the pain could be undetermined. Another patient could also be diagnosed with all of those same conditions yet experience no symptoms.
The following sections explore specific factors that may be involved in pain occurring in the various structures of the cervical spine.
How the Disc Itself May Become Painful
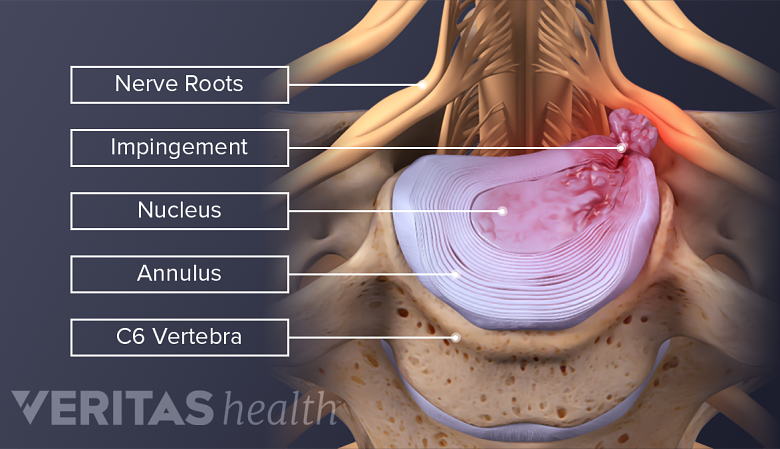
Inflammatory proteins from the inner core of the disc can inflame the nerve, causing pain.
The disc’s inner layer (nucleus pulposus) does not contain nerves and is not thought to become painful. However, there is some innervation in the outer part of the disc (annulus fibrosis).
The outer part of the disc may become painful if:
- It experiences a tear in/near the nerves or
- The nucleus pulposus (which contains inflammatory proteins) seeps onto these nerves through tears in the annulus fibrosis.
See How a Disc Becomes Painful
As the annulus fibrosis gets more tears, scar tissue eventually forms and the nerves are more likely to grow deeper into the disc and come into contact with inflammatory proteins of the nucleus pulposus. According to one theory, these newly-formed scars and nerves might also be at increased risk for becoming chronically painful in some people but not others.
How the Facet Joint Itself May Become Painful
Worn cartilage in the facet joint can lead to bone grinding, inflammation, and pain.
When the facet joint is the source of pain, it is commonly called facet joint syndrome. The cervical facet joints are thought to be one of the more common sources of chronic neck pain.
See Symptoms and Diagnosis of Facet Joint Disorders
There is a delicate balance within each facet joint for optimal mechanical functioning. Anything that causes the two opposing bones (articular processes) within the joint to become misaligned—such as cartilage damage or changing load patterns from a degenerating spine—can disrupt the facet joint’s smooth mechanical functioning. Some potential sources of pain include:
- Increased stress on the joint capsule and synovial lining, which could get more tears. In addition to tears causing pain, this could lead to less synovial fluid being in the joint, resulting in less lubrication and nourishment for the protective cartilage, or more synovial fluid in response to inflammation, distending the facet capsule and causing pain.
- As cartilage wears away, bone starts to rub against bone, promoting inflammation and possibly pain.
See Treatment Options for Facet Joint Disorders
Cervical facet joint degeneration is usually due to cervical osteoarthritis.
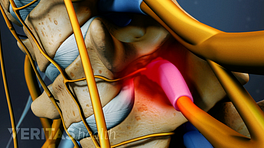
How the Nerve Root Itself May Become Symptomatic
Bone spurs can cause arm pain, weakness, and numbness by compressing nerves.
Anything that causes a nerve root to become compressed or inflamed can potentially lead to cervical radiculopathy symptoms of pain, tingling, numbness, and/or weakness radiating down into the shoulder, arm, and/or hand. In the cervical spine, common causes include:
- Herniated disc with inflammatory proteins leaking onto nerve root, or physical compression of the nerve root
- Bone spur growth compressing nerve root from nearby facet joint or uncovertebral joint
- Structural changes that narrow the foramen (opening where nerve root exits the spinal canal), such as loss of disc height and/or facet joints becoming misaligned
- Ligamentum flava thickening and pushing against nerve root
See Spinal Cord and Spinal Nerve Roots
However, the amount of nerve root compression/inflammation required to trigger cervical radiculopathy symptoms can vary significantly from person to person.
See Radiculopathy, Radiculitis and Radicular Pain
Similarly, the spinal cord can become dysfunctional and symptomatic (cervical stenosis with myelopathy) if it is compressed or inflamed by spinal degeneration.
See Spinal Cord Compression and Dysfunction from Cervical Stenosis
Other Structures That Can Become Painful as Cervical Spine Degenerates
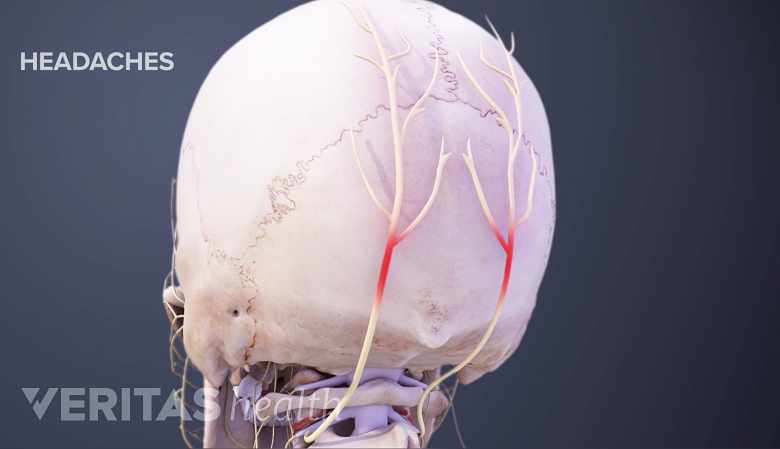
In rare cases, abnormal bone growth in the neck can cause headaches by affecting blood flow.
As facet joints and discs degenerate in the cervical spine, the increased inflammation and stress on the spine can potentially cause pain and symptoms in several other nearby tissues, such as muscles, ligaments, tendons, and vertebral arteries. For example, in rare cases degenerative boney overgrowth can push against a vertebral artery and affect blood flow, which could result in headaches, dizziness, or other serious problems.
- 1 Teraguchi M, Yoshimura N, Hashizume H, et al. Prevalence and distribution of intervertebral disc degeneration over the entire spine in a population-based cohort: the Wakayama Spine Study. Osteoarthr Cartil. 2014; 22(1):104-10