Piriformis syndrome typically develops after a direct injury to the buttock area or from repetitive trauma to the piriformis muscle due to excessive physical activity or poor posture—which makes the piriformis weak, tight, overused, or inflamed.
The muscle may also become a source of pain in the buttock and thigh due to anatomical causes, infection, or degenerative changes in the pelvic bones.
In This Article:
Common Causes of Piriformis Syndrome
The most common causes for piriformis muscle pain are when the muscle spasms, becomes tight, or increases in volume or mass (muscle hypertrophy).1Grgić V. [Piriformis muscle syndrome: etiology, pathogenesis, clinical manifestations, diagnosis, differential diagnosis and therapy]. Lijec Vjesn. 2013;135(1-2):33-40. https://pubmed.ncbi.nlm.nih.gov/23607175/ These changes may occur due to one or more of the following reasons:
- Trauma. Trauma to the hip or buttock area from a fall or direct injury can cause the piriformis muscle to become tight or inflamed, leading to pain, swelling, and muscle spasms. The muscle may also become strained or injured due to muscle imbalances or weakness, such as when one leg is stronger or more flexible.2Benson ER, Schutzer SF. Posttraumatic piriformis syndrome: diagnosis and results of operative treatment. J Bone joint Surg Am. 1999.81:941-949. https://pubmed.ncbi.nlm.nih.gov/10428125/,3Babu A, Gupta A, Sharma P, Ranjan P, Kumar A. Blunt traumatic superior gluteal artery pseudoaneurysm presenting as gluteal hematoma without bony injury: A rare case report. Chin J Traumatol. 2016.19(4):244-246. http://doi.org/10.1016/j.cjtee.2015.11.018
- Overuse. Piriformis syndrome can be caused by muscle overuse, such as repetitive movements from running or cycling or prolonged periods of sitting. When the piriformis muscle is used frequently or for extended periods, it can become strained and inflamed, leading to muscle spasms and pain.4Roy BA. Piriformis Syndrome. ACSM’s Health & Fitness Journal. 2014.18(4):3-4 http://doi.org/10.1249/FIT.0000000000000055
- Poor posture. Poor posture can lead to imbalances in the hip and pelvis muscles, which can cause the piriformis muscle to become tight or strained. Poor posture typically results from various factors, including muscle weakness, muscle imbalances, and poor muscle control.5Hicks BL, Lam JC, Varacallo M. Piriformis Syndrome. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448172/#_NBK448172_pubdet_
It is important to note that piriformis syndrome can also develop from a combination of these causes and if left untreated, can gradually increase the severity of symptoms.
Less Common Causes of Piriformis Syndrome

Anatomic variations of the sciatic nerve may increase the risk of piriformis syndrome.
Rarely, piriformis syndrome may develop due to degenerative changes in the spine or infection.
Less common causes of piriformis syndrome include:
- Anatomical variation of the sciatic nerve. It is estimated that around 16% of the population may have variations in the anatomical structure of the sciatic nerve relative to the piriformis muscle. In these individuals, the nerve may divide above the piriformis; pass above, below, or through the piriformis; or exit from behind the muscle; increasing the risk of developing piriformis syndrome through the entrapment of the sciatic nerve.6Poutoglidou F, Piagkou M, Totlis T, Tzika M, Natsis K. Sciatic Nerve Variants and the Piriformis Muscle: A Systematic Review and Meta-Analysis. Cureus. 2020;12(11):e11531. Published 2020 Nov 17. http://doi.org/10.7759/cureus.11531,7Davis D, Vasudevan A. Sciatica. [Updated 2019 Feb 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507908/Watch Sciatic Nerve Anatomy Video
- Degenerative changes in the spine: Degenerative spinal changes, such as a herniated disc or spinal stenosis, can irritate or compress the sciatic nerve, causing sciatica and, over time, leading to irritation and inflammation of the piriformis muscle. These degenerative changes can occur because of aging, injury, or other underlying conditions, such as osteoarthritis.1Grgić V. [Piriformis muscle syndrome: etiology, pathogenesis, clinical manifestations, diagnosis, differential diagnosis and therapy]. Lijec Vjesn. 2013;135(1-2):33-40. https://pubmed.ncbi.nlm.nih.gov/23607175/
- Infection (pyomyositis). Rarely, piriformis syndrome can be caused by a bacterial or fungal infection in the piriformis muscle or surrounding tissue(s). Other symptoms, such as fever and swelling, typically accompany piriformis infection.8Siddiq MAB, Rasker JJ. Piriformis pyomyositis, a cause of piriformis syndrome-a systematic search and review. Clinc Rheumatol. 2019.38(7):1811-1821. http://doi.org/10.1007/s10067-019-04552-y
-
If piriformis syndrome is suspected, it is advisable to consult a physician, who can evaluate the health of the lower back and pelvic tissues in detail to rule out serious conditions and accurately diagnose piriformis syndrome.
Risk Factors for Piriformis Syndrome

A wider pelvis in women makes them more susceptible to piriformis syndrome.
Certain risk factors may increase the likelihood of developing piriformis syndrome. A few examples include2Benson ER, Schutzer SF. Posttraumatic piriformis syndrome: diagnosis and results of operative treatment. J Bone joint Surg Am. 1999.81:941-949. https://pubmed.ncbi.nlm.nih.gov/10428125/:
- Occupation. Individuals with jobs requiring prolonged periods of sitting, such as office work and truck drivers, may be at increased risk of developing piriformis syndrome.
- Athletes. Athletes who participate in sports that involve running or cycling, or activities that involve repetitive hip or thigh motions, such as soccer, tennis, and basketball, may be at increased risk of developing piriformis syndrome due to muscle overuse.
- Age. The likelihood of developing piriformis syndrome increases as a person gets older, and it is more common in middle-aged people in the age group of 30-40 years.4Roy BA. Piriformis Syndrome. ACSM’s Health & Fitness Journal. 2014.18(4):3-4 http://doi.org/10.1249/FIT.0000000000000055
- Gender. Women are up to 6 times more likely to develop piriformis syndrome than men due to a wider pelvic bone.3Babu A, Gupta A, Sharma P, Ranjan P, Kumar A. Blunt traumatic superior gluteal artery pseudoaneurysm presenting as gluteal hematoma without bony injury: A rare case report. Chin J Traumatol. 2016.19(4):244-246. http://doi.org/10.1016/j.cjtee.2015.11.018,9Boyajian-O'Neill LA, McClain RL, Coleman MK, Thomas PP. Diagnosis and Management of Piriformis Syndrome: An Osteopathic Approach. Journal of Osteopathic Medicine. 2008.108(11):657-664. https://doi.org10.7556/jaoa.2008.108.11.657
- Previous injury. A prior injury to the hip or buttock area, such as a fall or blunt trauma, may cause piriformis syndrome to develop if the injury doesn't heal properly over time.10Vij, N. Kiernan H, Bisht R, et al. Surgical and Non-surgical Treatment Options for Piriformis Syndrome: A Literature Review. Anesth Pain Med. 2021.11(1):e112825. http://doi.org/10.5812/aapm.112825
- Physical inactivity. People with a sedentary lifestyle and little or no physical activity are more likely to develop piriformis syndrome due to weakness and inflexibility in the hip and gluteal muscles.9Boyajian-O'Neill LA, McClain RL, Coleman MK, Thomas PP. Diagnosis and Management of Piriformis Syndrome: An Osteopathic Approach. Journal of Osteopathic Medicine. 2008.108(11):657-664. https://doi.org10.7556/jaoa.2008.108.11.657
- Obesity. People who are overweight or obese have an increased risk of developing piriformis syndrome due to increased pressure on the muscle.
The presence of one or more of these risk factors does not guarantee that a person will develop piriformis syndrome, but when combined with the individual’s age and general health, they may increase the likelihood of developing the condition.
Activities That Cause Piriformis Syndrome Symptoms to Flare Up
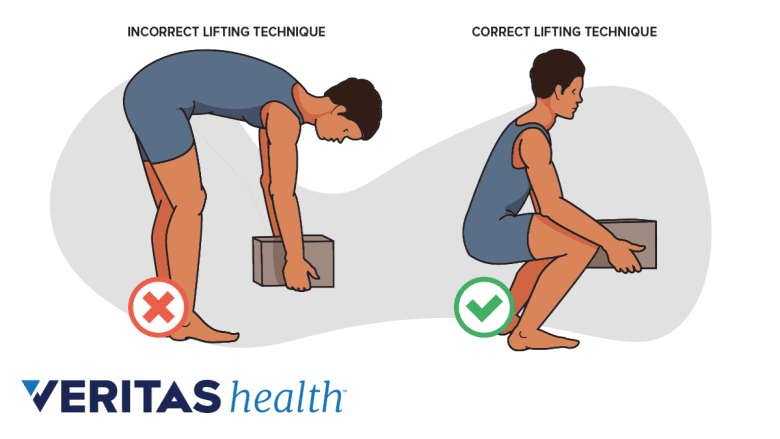
Incorrect lifting techniques can flare piriformis muscle pain.
When experiencing symptoms of piriformis syndrome, it is important to avoid certain activities, which may cause the symptoms to flare. A few common activities and their effects on the piriformis muscle are described below11Heiderscheit B, McClinton S. Evaluation and Management of Hip and Pelvis Injuries. Physical Medicine and Rehabilitation Clinics of North America. 2016.27(1):1-29. http://doi.org/10.1016/j.pmr.2015.08.003:
- High-impact activities, such as running or jumping, can place excessive stress on the piriformis muscle and result in its overuse.
- Prolonged sitting or standing can cause the piriformis muscle to tighten or spasm, worsening the symptoms.
- Repetitive twisting or rotating of the hips from playing sports such as golf or tennis can strain the piriformis muscle.
- Lifting or carrying heavy objects can put increased pressure on the piriformis muscle and worsen the symptoms.
- Intense cycling for long distances, especially if the seat position is not set too high or too low, can make the piriformis muscle fatigued due to higher stress.
Repeated microtrauma to the piriformis muscle from these activities can cause the pain to flare immediately and worsen over time, resulting in chronicity.
It is advisable to see a doctor if symptoms of piriformis syndrome are experienced. Piriformis syndrome typically improves if treated early and may become chronic and more severe if left untreated.
- 1 Grgić V. [Piriformis muscle syndrome: etiology, pathogenesis, clinical manifestations, diagnosis, differential diagnosis and therapy]. Lijec Vjesn. 2013;135(1-2):33-40. https://pubmed.ncbi.nlm.nih.gov/23607175/
- 2 Benson ER, Schutzer SF. Posttraumatic piriformis syndrome: diagnosis and results of operative treatment. J Bone joint Surg Am. 1999.81:941-949. https://pubmed.ncbi.nlm.nih.gov/10428125/
- 3 Babu A, Gupta A, Sharma P, Ranjan P, Kumar A. Blunt traumatic superior gluteal artery pseudoaneurysm presenting as gluteal hematoma without bony injury: A rare case report. Chin J Traumatol. 2016.19(4):244-246. http://doi.org/10.1016/j.cjtee.2015.11.018
- 4 Roy BA. Piriformis Syndrome. ACSM’s Health & Fitness Journal. 2014.18(4):3-4 http://doi.org/10.1249/FIT.0000000000000055
- 5 Hicks BL, Lam JC, Varacallo M. Piriformis Syndrome. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448172/#_NBK448172_pubdet_
- 6 Poutoglidou F, Piagkou M, Totlis T, Tzika M, Natsis K. Sciatic Nerve Variants and the Piriformis Muscle: A Systematic Review and Meta-Analysis. Cureus. 2020;12(11):e11531. Published 2020 Nov 17. http://doi.org/10.7759/cureus.11531
- 7 Davis D, Vasudevan A. Sciatica. [Updated 2019 Feb 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507908/
- 8 Siddiq MAB, Rasker JJ. Piriformis pyomyositis, a cause of piriformis syndrome-a systematic search and review. Clinc Rheumatol. 2019.38(7):1811-1821. http://doi.org/10.1007/s10067-019-04552-y
- 9 Boyajian-O'Neill LA, McClain RL, Coleman MK, Thomas PP. Diagnosis and Management of Piriformis Syndrome: An Osteopathic Approach. Journal of Osteopathic Medicine. 2008.108(11):657-664. https://doi.org10.7556/jaoa.2008.108.11.657
- 10 Vij, N. Kiernan H, Bisht R, et al. Surgical and Non-surgical Treatment Options for Piriformis Syndrome: A Literature Review. Anesth Pain Med. 2021.11(1):e112825. http://doi.org/10.5812/aapm.112825
- 11 Heiderscheit B, McClinton S. Evaluation and Management of Hip and Pelvis Injuries. Physical Medicine and Rehabilitation Clinics of North America. 2016.27(1):1-29. http://doi.org/10.1016/j.pmr.2015.08.003

